NIMH-Funded Research Highlights Effective Strategies to Reduce Suicide Attempts Among Adult Primary Care Patients
• Research Highlight
Suicide remains one of the most significant causes of mortality in the United States, posing a considerable public health challenge. Numerous studies have established that identifying individuals at risk for suicide during routine healthcare appointments can significantly mitigate potential tragedies. Primary care settings are particularly crucial in this effort, as research reveals that over 40% of individuals who died by suicide had visited their primary care provider within the month prior to their death. This indicates the vital role that these healthcare environments play in suicide prevention.
A groundbreaking study funded by the National Institute of Mental Health (NIMH) demonstrated that the incorporation of targeted suicide care practices during routine primary care appointments led to a 25% reduction in suicide attempts within three months following these visits. This compelling evidence underscores the importance of empowering primary care clinics to actively engage in suicide prevention measures, thus fostering a more integrated approach to mental health care within the healthcare system.
Understanding the Research Methodology and Approach Used in the Study
During most healthcare visits, primary care clinicians routinely screen for depression, often including inquiries about potential suicide risk. Prior research supported by NIMH indicated that utilizing screening tools for suicidal thoughts, coupled with brief safety planning, can effectively diminish the likelihood of suicide attempts. This study, spearheaded by Dr. Julie Angerhofer Richards at the Kaiser Permanente Washington Health Research Institute, sought to evaluate whether the integration of suicide care practices into standard adult primary care visits could indeed lead to a decrease in subsequent suicide attempts.
This research analyzed secondary data from a broader integrated study examining the National Zero Suicide Model, which is the first program in the United States linked to a significant reduction in suicides among behavioral health patients. The research team had previously explored this model in a different NIMH-funded study conducted across six health systems nationwide.
Initially, caregivers provided standard care, which did not encompass systematic suicide screening or follow-up protocols. A total of 22 clinics were randomly assigned to implement suicide care practices on staggered timelines (spaced 4 months apart) over a two-year period. Throughout the study, more than 333,593 patients attended over 1.5 million primary care appointments, providing a substantial data pool for analysis.
The components of suicide care included:
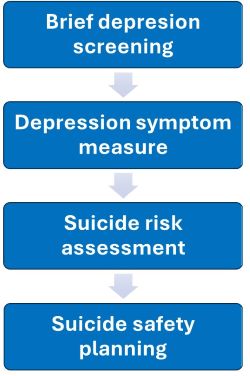
- Depression screening: Every patient underwent a brief two-question depression screener, and those who scored positively on either question were administered a more comprehensive depression symptom scale.
- Depression symptom scale: The initial screener was followed by an extensive depression symptom measurement for patients who indicated positive responses.
- Suicide risk assessment: Patients expressing thoughts of self-harm or suicide were required to complete a detailed evaluation of their suicidal thoughts and behaviors.
- Suicide safety planning: Patients reporting intent or plans for suicide within the previous month were referred to specialized care staff, including mental health social workers, for immediate safety planning. This safety planning process was collaborative, enabling patients and providers to identify warning signs, outline coping strategies, and create safe environments to manage suicidal crises.
Three vital strategies underpinned the intervention:
- Experienced facilitators conducted training sessions at each clinic and maintained ongoing support to address challenges and foster problem-solving.
- Clinical decision support integrated into the clinics’ electronic medical record systems provided pre-visit reminders and visit prompts to ensure compliance with screening protocols.
- Regular performance monitoring of medical records assessed clinician adherence to screening and assessment documentation standards.
Researchers compared the outcomes of clinics implementing suicide care with those providing standard care, focusing on:
- The documentation rates of suicide risk assessments and safety planning in the medical records within two weeks following an at-risk patient’s primary care visit
- The rates of suicide attempts or fatalities in the 90 days subsequent to their primary care appointments
Key Findings: The Impact of Integrating Suicide Care into Primary Care Practices
The integration of suicide care into regular adult primary care visits resulted in markedly elevated rates of suicide risk screening, assessment, and collaborative safety planning. This intervention ultimately contributed to a 25% decrease in suicide attempts within 90 days post-visit when compared to clinics that maintained usual care practices. These findings collectively illustrate that embedding suicide prevention strategies into adult primary care not only increases the screening of suicidal thoughts and behaviors but also leads to a significant reduction in subsequent suicide attempts.
This research aligns with NIMH’s commitment to prioritizing suicide prevention within healthcare settings, aiming to ultimately lower the overall suicide rate across the United States. The study highlights crucial next steps for healthcare providers and care teams in addressing suicidal ideation during clinical encounters, ultimately playing a vital role in saving lives.
Research Citation and Source Acknowledgment
Richards, J. A., Cruz, M., Stewart, C., Lee, A. K., Ryan, T. C., Ahmedani, B. K., & Simon, G. E. (2024). Effectiveness of integrating suicide care in primary care: Secondary analysis of a stepped-wedge, cluster randomized implementation trial. Annals of Internal Medicine, 177(11), 1471–1482. https://doi.org/10.7326/M24-0024
Access Critical Support for Mental Health Concerns
If you or someone you know is experiencing distress or having thoughts of suicide, please reach out to the 988 Suicide and Crisis Lifeline by calling or texting 988 or chatting online at 988lifeline.org . In emergencies, do not hesitate to call 911.
Explore Additional Resources for Suicide Prevention Strategies
Important Disclaimer Regarding the Zero Suicide Framework
The Zero Suicide framework was developed by the Education Development Center (EDC) through federal funding from the Suicide Prevention Resource Center and the National Action Alliance for Suicide Prevention. Information and branding related to Zero Suicide are available at no cost via the Zero Suicide ToolkitSM Here you can find the original article; the photos and images used in our article also come from this source. We are not their authors; they have been used solely for informational purposes with proper attribution to their original source.













