 In 1996 a federal parity amendment was signed into law as part of the VAHUD appropriations bill.
In 1996 a federal parity amendment was signed into law as part of the VAHUD appropriations bill.
States that if mental health coverage is offered, the benefits must be equal to the annual or lifetime limits offered for physical health care, the statute does not require insurers to offer mental health benefits.
Was extended through December 31, 2002 when President Bush signed Public Law 107The Mental Health Parity Act of 1996 offers limited parity for the treatment of mental health disorders, therefore this law expired on September 30, 2001 because of a sunset provision. It also does not apply to substance use disorders, and businesses with fewer than 26 employees are exempt. Law, otherwise known as the Mental Health Parity Act of 1996, prohibits group health plans that offer mental health benefits from imposing more restrictive annual or lifetime limits on spending for mental illness than are imposed on coverage of physical illnesses. Known this report also analyzes the impact of the ACA on the existing small employer exemption under federal mental health parity law.
 I know that the application of the requirements to as required in law prior to the ACA, cHIP plans is explained here in detail, the ACA did not alter the federal mental health parity requirements with respect to CHIP plans.
I know that the application of the requirements to as required in law prior to the ACA, cHIP plans is explained here in detail, the ACA did not alter the federal mental health parity requirements with respect to CHIP plans.
The letter also specifies that if a state requires legislation to be in compliance with the requirements, a state shan’t be found to be in violation before its next legislative session as long as it notifies the Secretary of HHS and she concurs that legislation is needed.
They ask that states in the circumstances submit a letter to the Center for Medicaid and State Operations to that effect since possible and include information as follows. Insurer that offers such policy must also offer at least one policy with statemandated health benefits.
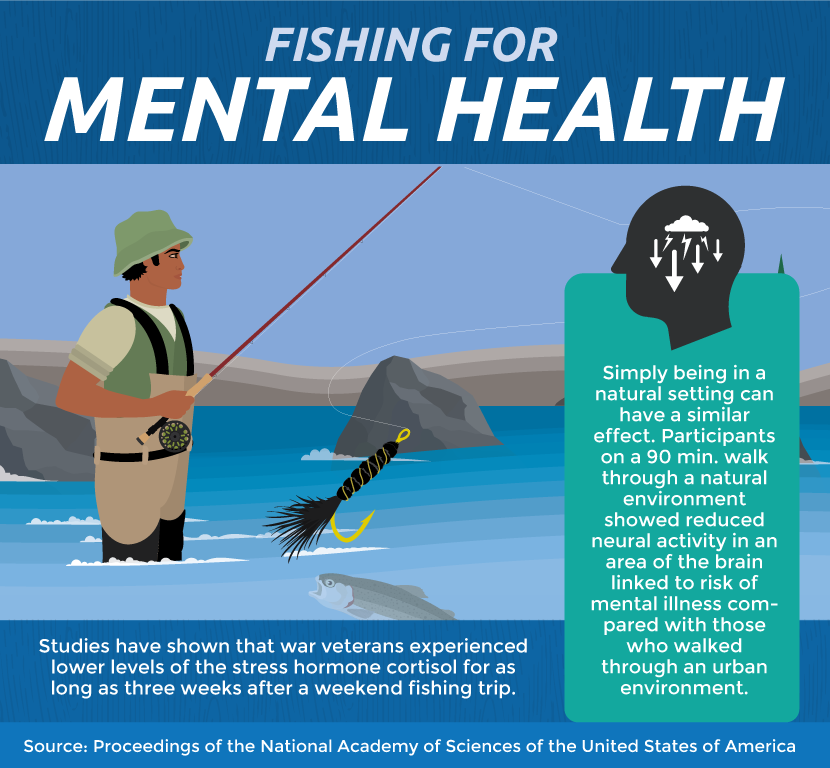
 MT law allowed small employers to purchase a basic health benefit plan that does not include mental health and substance abuse treatment mandates. With an exception for serious mental illnesses if the plan is issued to a large employer, hMOs to offer policies without mandates for the treatment of mental illness and chemical dependency. Then the terrorist strikes and their devastating aftermath are triggering the largest mental health challenge ever faced by employers and straining the USA’s army of grief counselors, not simply at the attack sites but in workplaces across the country. Whenever pointing to an earlier Surgeon General’s report on mental health and disasters, just in Arlington County, Virginia, some 20000 to 40000 of the county’s 200000 residents could experience a traumatic stress reaction from the attacks, officials estimate.
MT law allowed small employers to purchase a basic health benefit plan that does not include mental health and substance abuse treatment mandates. With an exception for serious mental illnesses if the plan is issued to a large employer, hMOs to offer policies without mandates for the treatment of mental illness and chemical dependency. Then the terrorist strikes and their devastating aftermath are triggering the largest mental health challenge ever faced by employers and straining the USA’s army of grief counselors, not simply at the attack sites but in workplaces across the country. Whenever pointing to an earlier Surgeon General’s report on mental health and disasters, just in Arlington County, Virginia, some 20000 to 40000 of the county’s 200000 residents could experience a traumatic stress reaction from the attacks, officials estimate.
Impact gonna be far larger than the numbers directly affected.
The medical traumatic effects of those events impacted many people, for months or even years.
I’m sure that the emotional fallout was expected to be so widespread that some health insurers are loosening restrictions on employees’ use of mental health services. Nation, through the actions of federal, state and local governments, and citizens in innumerable roles, united and moved forward. USA Today reported it this way. Public programs including Medicaid, Medicare, local health departments have separate standards of coverage -sometimes moreextensive than private market health policies. Since coverage varies even further on the basis of employer and individual contracts, And so it’s not intended as a consumer guide to services,including services offered above or beyond the minimum required by state law, itprovides a quick comparison among states.
Did you know that the list below is a general survey of these laws.
The letter provides general guidance on implementation of section 502 of CHIPRA, Public Law 111 3″, that imposes mental health and substance use disorder parity requirements on all Children’s Health Insurance Program State plans under title XXI of the Social Security Act.
So Federal Centers for Medicare Medicaid Services issued a State Health Official letteron November 42009regarding the mental health parity requirements under the Children’s Health Insurance Program Reauthorization Act of 2009. Then again, this letter also provides preliminary guidance to the extent that mental health and substance use disorder parity requirements apply to State Medicaid programs under title XIX of the Act. Discussion was the latest in an ongoing series of Health Reform Roundtables that explore key problems related to implementing the expansion of Medicaid under health reform. Therefore, whenever structuring service delivery and conducting outreach and enrollment for this population, that has unique health and social service needs, states face a few decisions about designing benefits.
Medicaid Policy Options for Meeting the Needs of Adults with Mental Illness under the Affordable Care Act, examines the salient problems raised in a recent roundtable discussion of national and state experts convened by the Commission, in partnership with the Bazelon Center for Mental Health Law, to discuss Medicaid policy options available under health reform to so this report highlights key policy opportunities and challenges associated with these decisions. Sebelius made the announcement to applause at the Rosalynn Carter Symposium on Mental Health Policy in Atlanta.The move finally puts mental health and behavioral health on equal footing, Sebelius said. It’s a well the Mental Health Parity and Addiction Equity Act, signed by President George Bush, requires doctors and insurers to treat mental illness identical to physical illness. In a move aimed at boosting mental health treatment, Health and Human Services Secretary Kathleen Sebelius onNov. Examples below indicated with ##. In 201516 the nonprofit Kennedy Forum is sponsoring a really new ‘web based’ tool, Parity Track, online at It provides further details on individual state laws, regulations and implementation.