Quartet offers a program that can bring behavioral and physical health gether in one streamlined process.
Quartet offers a program that can bring behavioral and physical health gether in one streamlined process.
That’s not always a reliable method.
Commonly, the way a provider gathers information about a patient’s other care is simply through asking them during an appointment. Anyways, quartet advertises that it could save as much as $ 10 per month per member. Ruktanonchai said the decision to expand needs to be on the basis of more than dollars and cents. Actually the focus can turn to another big issue that can lessen thequality of care for patients with both physical and behavioral health problems, with a patient flowing from one system to the other. Through the Quartet system, the patient’s medical records are passed from the primary care physician’s office to the mental and behavioral health provider, and vice versa. That means the insurance company working with Quartet, that in this case is Highmark, is covering more mental health visits and spending more money. So, kennedy called it a value proposition to spend more on mental health as long as the savings are seen in the treatment of physical health.
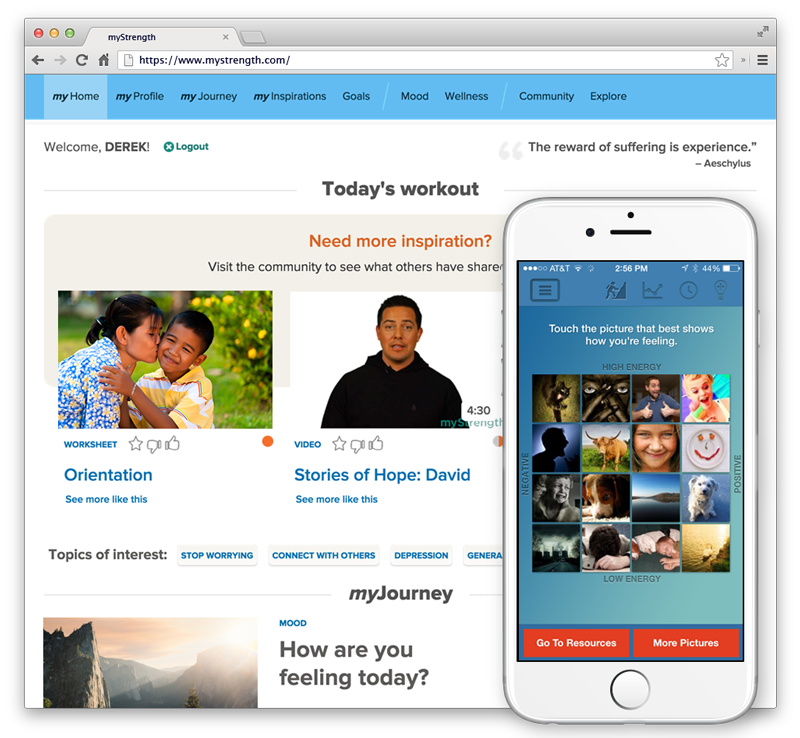 Primary care doctor can therefore make sure that the patient is following their treatment course and make sure if there’re there any changes that need to be made.
Primary care doctor can therefore make sure that the patient is following their treatment course and make sure if there’re there any changes that need to be made.
Most mental and behavioral health patients first get as a matter of fact, more prescriptions for antidepressants drugs are written by primary care physicians than by mental health doctors. Notice that highmark rolled out Quartet in June, in six western Pennsylvaniacounties including Allegheny.The insurance provider is evaluating the outcomes of the first a couple of months and will decide whether to expand use to other parts of itsservice area. Make sure you write a few comments about it. The system is designed to send the patient to the mental health provider who can best serve their needs.
Thanks to an 8 year old federal law, insurance companies must offer benefits for mental health treatments that are substantially almost identical to the benefits for medical or surgical treatments.
That does not always mean patients are actually getting the behavioral and mental health servicesthey need, even when they get the right diagnoses.
Insurance companies need to look beyond instant savings and at the bigger picture, he said.
Those savings gonna be far off, Kennedy said. While arguing that behavioral and mental health care needto be a part of treating physical ailments like heart disease, diabetes and cancer, on the board, he spends time making the financial argument for more treatment. Eventually, it turns into a blackish box, Ruktanonchai said, only after a doctor makes the diagnosis.