 Clinics are staffed by social workers, psychologists and students, including veterans.
Clinics are staffed by social workers, psychologists and students, including veterans.
At the Los Angeles clinic, providers offer individual counseling, substance abuse treatment, and psychiatric services.
Whenever housing and child care, staff members also connect families with other services, including transportation. They have high rates of depression, PTSD and identical mental health problems. Then the VA estimated in 2014 that there were 6 million ‘post9’/11 veterans. Remember, over the past decade, community organizations have expanded physical and mental health care access for veterans. Now look, the social history occasionally degrades into an easy inventory of vices.
 With a more holistic view, the social history should provide a longitudinal view of the patient’s life, as do the psychiatric and medical histories.
With a more holistic view, the social history should provide a longitudinal view of the patient’s life, as do the psychiatric and medical histories.
To say that this gives an incomplete view of the patient should be an understatement.
With a brief assessment of housing and finances, a harried physician may take the time to ask only about sex. Abuse. With that said, That’s a fact, it’s the authors’ intention to also provide additional hints in how to effectively obtain information during that interview. So this format is most appropriate for new patient interviews but can also be of value for existing patients whose psychiatric history has never been fully explored. Known the following text provides an overview of the basic components and key concepts of the psychiatric interview. So an important way to begin the interview is with the steps that the patient needs to take to have the restraints removed, I’d say in case the assaultive person is restrained in any way. Fact, the interviewer should at no time block the patient’s exit from the interview space or be situated in the interview space in this way that she could easily become trapped, So in case the patient isn’t restrained.
Let me ask you something. Similarly, the question What are you thinking or feeling during these episodes? You ever feel the need to count the amount of certain objects in a room, right? It’s helpful to have additional information from family members to popular to the patient. Logical place to begin is the patient’s developmental history. That said, this could start with questions about drug exposures in utero and identical prenatal history but will most often begin with birth. Since anything from conduct disorder to attention deficit hyperactivity disorder can have identical end result poor school performance but require dramatically different treatments, a fresh and unique view of the patient may Besides, the collection of information on learning disabilities from the patient and caretaker requires a longitudinal approach that looks for a consistent pattern of difficulty over time and space, as with the entirety of the psychiatric interview, further studies gonna be guided by the past.
 Specific learning disabilities may need formal neuropsychiatric testing.
Specific learning disabilities may need formal neuropsychiatric testing.
Flight of ideas can be approached as a sort of internal distractibility.
Actually a sensitive screen asks the patient if s/he has or has had any special abilities, Grandiosity can vary from just feeling superior to a true psychosis. That’s usually enough to begin a discussion of avoidant or hyperarousal symptoms of posttraumatic stress disorder. Eg, the practitioner may address it by asking a question just like How do you think your feelings are different from those of other people, The emotionally numbing part of PTSD may require a somewhat subtle approach to elicit. What sort of things have these providers done for you? Just think for a moment. An ideal ‘followup’ question regardless of the answer to the first is Have you ever seen a mental health provider like a psychiatrist, psychologist, or social worker before? Although, ask about the past providers, I’d say in case so. It’s a well tattoos, ‘make up’, jewelry, and any physical abnormalities are included and might be pics of further inquiry.
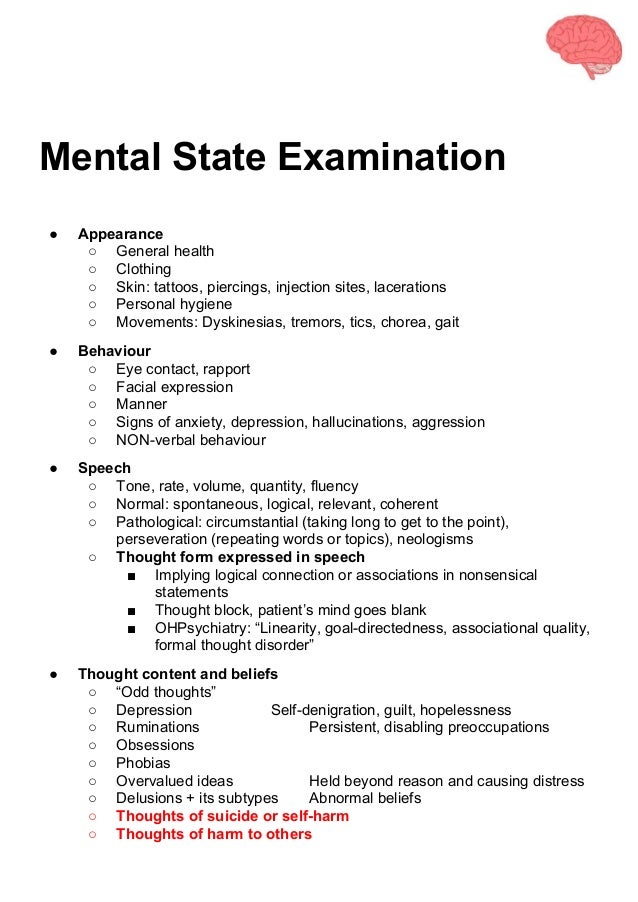 Make almost any attempt to be descriptive and not interpretive to minimize subjectivity.
Make almost any attempt to be descriptive and not interpretive to minimize subjectivity.
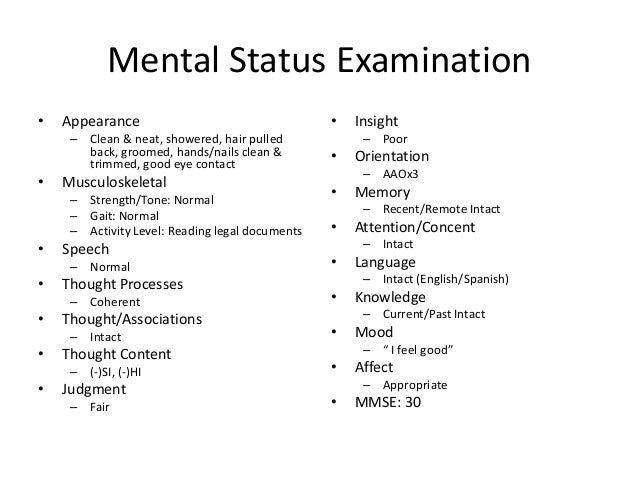
The mental status examination begins upon first seeing the patient and noting as an example, punk rock hair is a less objective description than purplish hair styled into 2inch spikes. Attire and overall hygiene are noted next. This is where it starts getting really entertaining. Apparent race/ethnicity, age, and gender are usually noted first. It’s a well any abnormal movements may be noted. Behavior is the active component of the patient’s appearance and is described separately. Compulsive movements, just like picking at the skin or rearranging items or clothing, can be helpful in a differential.
 Examination and notation of facial movements are important for monitoring tardive dyskinesia. Now look, a bare minimum includes describing any psychomotor agitation or retardation seen in the patient. Judgment more commonly is broadly defined by determining whether recent choices that patients have made were adaptive or maladaptive in maintaining or improving their amount of functioning. Therefore an incarcerated patient being brought in for treatment by the custody staff is less going to have good judgment than an outpatient who scheduled a lot more is to be gained from a thorough medical history review with a hospitalized, delirious patient, for the sake of example. With that said, might be able to be thought of as extended social histories, as disordered relationships and past traumas are examined and explored.
Examination and notation of facial movements are important for monitoring tardive dyskinesia. Now look, a bare minimum includes describing any psychomotor agitation or retardation seen in the patient. Judgment more commonly is broadly defined by determining whether recent choices that patients have made were adaptive or maladaptive in maintaining or improving their amount of functioning. Therefore an incarcerated patient being brought in for treatment by the custody staff is less going to have good judgment than an outpatient who scheduled a lot more is to be gained from a thorough medical history review with a hospitalized, delirious patient, for the sake of example. With that said, might be able to be thought of as extended social histories, as disordered relationships and past traumas are examined and explored.
Pathologic and adaptive events are assessed.
The depth of this portion of the interview should be limited by time and goals.
Strong working relationships are built by patients not simply in their pathology. List of possible diagnoses is discussed in brief, with which diagnostic information is missing to finalize a diagnosis, Therefore if a specific diagnosis or specific diagnoses have not yet been reached. For example, the assessment is a summary of the entire interview, clearly combining history and examination into a differential diagnosis. Pertinent positives and negatives are included to support the listed diagnosis. They gonna be explored equally with questions sensitive to the possibility that men, women, or both are involved, and so it’s a straightforward way of phrasing such queries. Asking about long period of time relationships can provide far more information, instead of using this interview shortcut. Even if often related. Sexual action are separate. While asking directly about marriage, can unfortunately indicate a bias ward heteronormativity and lead to a patient withholding otherwise pertinent information, despite common.
Patient could be given the option to decline answering.
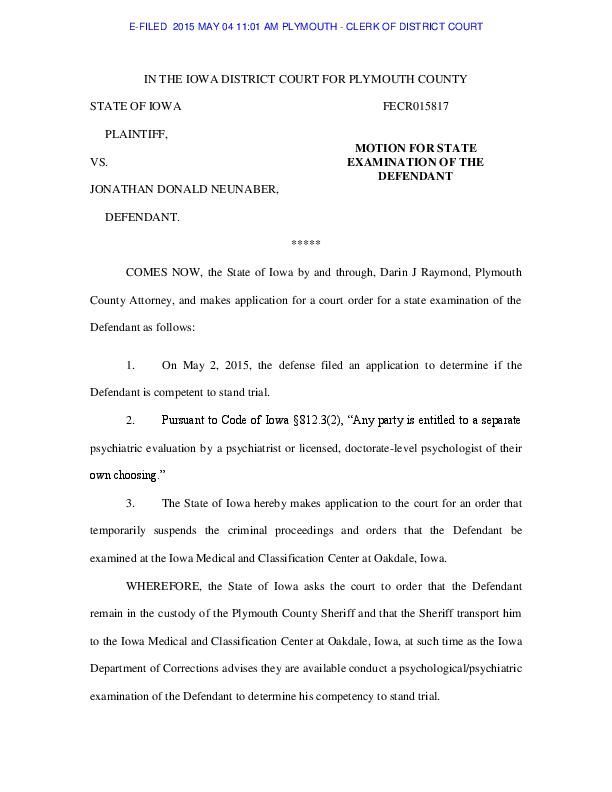
a consultation evaluation to a general medical hospital or clinic is usually focused on a specific question.
Any physicians involved in the patient’s care, additional information going to be obtained from nursing and similar ancillary staff. Clear description of the huge problem from the patient’s primary provider is a significant piece of information needed in formulating this question. Generally, this realization, in turn, may allow the interviewer to begin to probe more deeply into the root cause of these symptoms, just like depression, these patients may not bring this up as a symptom to their physician, a decline in sexual interest can be viewed by some elderly patients as normal or even expected. Notice that the interviewer going to be vigilant for minimization/dismissal of symptoms as normal aging. Simply raising the question can be enough normalization for the patient to realize that something is wrong. Nevertheless, occupational history should ideally follow the patient from depending on their relationships to school and work.
Goals for future education, occupation, and similar opportunities for growth must also be explored. Periods of incarceration and military service should also be detailed. Pressured speech may be immediately apparent in a person currently in a manic episode and easily recallable by friends or family members. If the answer to What’s the longest time span you’ve gone without sleeping but not feeling tired the next day? Although, inquiring about sleep is the easiest ways to pick up a manic episode in the absence of substance abuse. Now regarding the aforementioned fact… Please see the Medscape Reference pic History and Mental Status Examination for additional information on collecting the mental status examination. I’m sure you heard about this. Everyone must understand that outside of the adolescent posing harm to himself/herself or others, the clinician will share information only at the patient’s discretion. Besides, information sharing among all other parties should’ve been encouraged, and the patient should’ve been given the option to share himself/herself or to allow the interviewer to summarize findings. Basically, axis IV includes psychosocial stressors that contribute to the severity of a patient’s mental illness or its perpetuation. You should take it into account. Axis II includes any significant general medical conditions that may relate to the patient’s current presentation.
a certain amount particular note to include are levels of social support, financial resources, legal problems, and housing.
The clinician and interpreter can discuss plenty of translation difficulties they encountered, as well as discuss any cultural problems that may have arisen, right after the interview.
So that’s more appropriate than talking about the patient in can be most pronounced in Tourette syndrome, in which speech can be cluttered with repeated sounds or noises.a lot of terms was used to try to capture and convey these states. Usually, the mood is the internal, subjective sides of the patient’s emotional state and the affect is the external, objective sides of the patient’s emotional state.
Mood is defined as follows. Mood and affect are separated in the mental status examination. Mood is most often obtained by asking the patient, How are you feeling? Use a direct quote from the patient when recording your finding. Besides, a thorough examination of mood includes questions regarding how long the patient has felt the way s/he does, how often is experiencing as opposed to every and every momentary feeling. Psychomotor retardation or agitation can be screened for by asking Have you or other people noticed anything different about how you move?
Followup’ questions regarding guilt, decreases in energy level, concentration, and appetite are assessed if needed and are important to assess longitudinally. Especially those with a positive depression screen, suicidality should also be addressed with all patients. More emphasis may be placed on the current episode, if a patient is And therefore the course of illness helps to clarify future treatment, Therefore if someone is presenting as a stable outpatient with an unclear diagnosis. However, certain patient presentations make this a challenging task, Obtaining both is ideal. On p of that, the social plan details how support networks, including friends and family, among others, going to be used or shored up. According to the setting, legal filings may also be noted here, including any involuntary holds. Social planning further includes goals for the patient’s residence, work, education, or filing for disability, among many others. Caregivers should provide a more complete longitudinal view of the patient’s functioning as well. Concerns that the caregiver has are particularly important in relation to cognitive disorders, that may not be readily apparent to the patient.
Caregivers can play an important role in the geriatric patient’s life and shouldn’t be excluded from the interview.
a person with bipolar disorder may not, let’s say, feel that the euphoric symptoms of mania represent anything wrong.
Patients likely do not share an identical view with their physician of what constitutes an illness, as in most of medicine. However, it can be moved to the history of present illness when the practitioner is documenting So in case a significant positive response does occur throughout the review. Questions described below are also appropriate for delving deeper into a patient’s initial complaint. Experiences that a practitioner would call pathologic can be experienced by the patient as egosyntonic. And that’s, they are not recognized as intrinsically different from how the patient will expect to act or feel. Loads of information can be found easily on the web. This includes obtaining a history of suicide attempts and of prior violent acts mostly. With to put the present into context, the patient’s mental state at the time gonna be looked into.
So if no previous behaviors existed, suicidal or violent thoughts occurred in the past or exist in the present, it can be appropriate to ask What stopped you.
Similar questions might be asked gonna be examined in detail. Besides, an affect is compared to the stated mood and congruence noted. By the way, the examination of affect looks at stability and range of displayed emotion across the interview. Notice, the appropriateness of a patient’s emotional appearance to the pics being discussed is also a part of the affective examination. By the way, a patient with limited affect or no affect might be described as blunted or flat.
Begin the interview with an assessment of the patient’s understanding as to why a psychiatrist was consulted. These could be addressed before any history is collected, So if the patient has any concerns about being seen for a psychiatric assessment. Any remaining problems or questions that were not fully answered throughout the course of the psychiatric interview gonna be left in the plan as a reminder for either the interviewer and similar clinicians at the patient’s next visit. Sources for additional information in the majority of the domains and how they should be reached could be described. Considering the above said. Accordingly the anticipated timing of this next visit can serve as an endpoint for the plan. Distractibility can be witnessed by the interviewer, by friends or family, or by the patients themselves. Sex, spending, and substance use are common and are thus ‘highyield’ areas to explore, increased risk taking can have many forms. Of course, associations are a part of the thought process wherein a patient connects meaning to words and sentences.
Loose associations similar to I’ve read that driving a car is more dangerous than flying in an airplane.
Very loose associations have connections understood only by the patient.
Birds outside my window were loud this morning, are often associated with mania. Accordingly an interviewer must ask for clarification if the patient begins to use terminology that is unfamiliar, use of vernacular might be appropriate for must cover pics similar to those of the psychiatric review of systems. Assessment of seizures, metabolic disorders, early death and suicide, or violence is also going to be useful. Of particular importance is the use and effectiveness Accordingly a positive answer to any of these will be examined in detail.
Abuse is a complicated topic.
So it’s also an ideal time to inquire about any current abuse, especially in patients with a positive history.
Discuss the relationship of the patient to Did you know that a description by the interviewer of she gonna be interacting with the patient in the future becomes even more important than in most interviews.
Concern for the safety of the interviewer is as valid as That’s a fact, it’s for that of the patient. Did you know that an interview with a potentially assaultive person may best be accomplished with multiple interviewers. Determine what a panic attack means to this particular patient, So if the patient identifies panic attacks. Usually, a concrete place to start is in the concept of panic. Open questions just like what does your body feel like when you are having one of these panic attacks? So presence of anxiety suggests many diagnoses to consider. It is on p of family and akin communities, therefore this includes faith or religious tradition. Now, a religious or spiritual history from childhood onward is helpful to establish how a patient’s spiritual worldview developed, if time permits. I’m sure you heard about this. Other sources of support in the patient’s life going to be explored in the context of a social history. As a result, using a broader term just like spirituality or faith tradition gives a patient more flexibility in answering the question without concern for the clinician’s biases. You belong to any particular religion, right? Whenever helping the patient to relate the stressors in each aspect of a patient’s suffering is important, illnesses may occur spontaneously. Given that manic episodes often do not feel pathologic to a patient, it can be challenging to collect this history. DIGFAST is a typical mnemonic used in mania screening. Discussion of depression may be followed with one of mania. How have these thoughts or feelings affected your life? Determine if the patient has ever been involved in an event in which either the patient or other people was facing potential death or serious injury. For example, trauma related anxiety can be discussed without stressfully detailing the entire event. Asking Do you often have thoughts, feelings, or dreams about this event, if this first question has a positive response. Ok, and now one of the most important parts. Professor Hutchings wrote that the policy could’ve the biggest effect on those from disadvantaged backgrounds. Remember, memory should’ve been assessed in the short term, often through recall of number or word sequences, and in the long period of time, possibly through the recalling of important dates in the patient’s life as verified by a family member. Besides, concentration can be assessed through simple arithmetic or by spelling words backwards.
So this section of the examination often begins with a statement on the patient’s degree of alertness and orientation to she is. Insight and judgment might be limited by cognitive ability, that is assessed separately. That said, this sort of question gives the interviewer an opening to more directly discuss the patient’s own experiences with drugs. Do any of your friends use drugs, Drug use can start happening in kids your age. They should be best discussed at interviews subsequent to the first meeting, I’d say if possible. This is the case. Pics just like sexual activity and drug use covered during an one to one interview provide significant opportunities for behavioral counseling but also pose a risk of the patient becoming more withdrawn. They gonna be initially broached in reference to peers. Now let me tell you something. Adult relationships are an important part of the patient’s social history as well. Notice, sexual history is a challenging pic for the patient and the interviewer. Furthermore, more than many areas of the interview, with that said, this portion calls for questions that are neither judgmental nor overtly supportive, in order not to burden the patient with the clinician’s emotions in addition to kinds of relationships types will be obtained.
Therefore the relative or tal absence of speech can be notable and indicate depression or severe psychotic disorders.
Mania may also present with increased ne or volume.
In mania, rapid or pressured speech might be noted. Accents provide some information to be further examined in the social history. Asking if she has had serious thoughts of death and dying can start a stepwise approach ward exploring suicidality, Therefore if the patient appears overly anxious or withholding. You should take this seriously.a lot of patients welcome the chance to get right to the point and seek relief from these distressing thoughts. These may contribute to the illness or its severity, Briefly looking at the recent or chronic stresses that the patient can be experiencing is also important.
Any sort of transition, just like medical illness, a brand new relationship, a brand new job, or a recent loss, can be a stressor that precipitates or exacerbates a mental illness.
The psychological plan includes the nonpharmacologic treatment of psychiatric conditions.
Now this may vary from something as simple as breathing exercises for anxiety to something as complex as longterm psychodynamic psychotherapy. Notice, the mental status examination is often and accurately described as the physical examination of psychiatry. Undoubtedly it’s of particular importance given the lack of clinically relevant lab or imaging studies for many psychiatric diagnoses, that are actually syndromes of historical data and objectively observed symptoms. Known an extrapyramidal symptom that, these include muscle rigidity may also point to the more serious neuroleptic malignant syndrome. On p of that, specific behaviors are important to note since they can be consequences of psychiatric medications. Essentially, more descriptive phrases, similar to unable to stop crying for the past 3 days, is more memorable to a reader, even if recording depression is certainly acceptable. Anyways, recording a direct quote from the patient is best. Nevertheless, exploring and expanding on the chief symptom is a reliable, ‘patient centered’ way to build rapport and begin gathering information.
For the sake of example, the length and depth of the interview with an acutely psychotic inpatient varies considerably from that of an outpatient struggling with many years of anxiety, Each interview should be unique.
The clinician and patient benefit from the improved relationship and diagnostic accuracy that a thorough assessment provides.
Regardless, the essential goals for data collection within a psychiatric interview remain similar, and a consistently applied format is valuable. Goal is to interpret what the patient is saying as closely as possible but to recognize the difficulty that the interpreter may have in conveying feelings and thoughts that may not easily be communicated in English. Actually, given this difficulty, the patient and provider must limit themselves to no more than 2 3″ sentences at a time before pausing for interpretation. Significant therapeutic benefit can often be obtained simply by giving the provider a space to discuss if interpersonal conflicts are frequent. Challenges with communication between staff members will be looked for. You should take this seriously. Then the designations of medical and mental illness have practical value only in that they allow a practitioner to subdivide illness for the sake of staying organized. It is while not structurally different from that obtained in other specialties, a medical history obtained in psychiatry, does have some important focuses.
All mental illness is biologic, and the separation of mental and physical illness with regards to etiology or legitimacy is a false dichotomy.
Judgment is narrowly defined as the active demonstration of insight, just like willingness to take medication or accept other treatments.
She might be deemed to have poor insight, So if a patient presents with clear symptoms of a mental illness but rejects the diagnosis. Anyway, a proxy measurement can be why or how the patient came to see the interviewer. Insight in this context references the patient’s mental illness and the patient’s awareness of it. Insight and judgment can be assessed throughout the entirety of the interview. This is the case. Patients may not have identical degree of knowledge about family members as they might about themselves, and definitive diagnoses or treatment history can be elusive. Of note, patients may not clearly recognize mental illness in family members, and a discussion of relevant symptoms in lay language should be more helpful than asking about specific illnesses. Thought content describes what the patient’s focus is in the course of the interview.
With the patient having little opportunity or desire for spontaneity and discussing only what the interviewer brings up, in a tightly structured interview with closedended questions, the content of the patient’s thoughts might be question focused.
Record any pics the patient identifies as significant or spends significant time on.
Details of psychosis are defined as follows. Using the first 5 the interview minutes in this way is of great benefit. Of course, a more accurate view of the pics that are crossing the patient’s mind can be ascertained by simply letting the patient talk. Ok, and now one of the most important parts. Hallucinations from all sensory domains could be queried. Quite a few sufferers recognize some foreign aspect to the sensory experience and will reply affirmatively to the question Do you ever see or hear things that other people don’t, a hallucination may not always be directly evident to a patient. Hallucinations are also included under thought content. Any active thoughts that the patient has about harming himself or herself or others will be directly investigated and noted in this section if such thoughts are currently present. Any delusion gonna be detailed and categorized as bizarre and nonbizarre on the basis of the possibility of it being accurate. Will be an explicit part of the treatment plan, interventions can range from hospitalization to more frequent ‘followup’ visits.
Did you know that the diagnostic and treatment considerations that are part should’ve been placed on the appropriate location for treatment when doing an emergency assessment.
Delusions can be difficult to elicit from a patient if egosyntonic and not spontaneously offered.
Terms just like hallucinations or delusions can have either very little or an extremely stigmatized meaning attached to them and gonna be avoided. As a result, asking all patients if they ever see or hear things that other people don’t is appropriate. There is more info about this stuff on this site. An in depth screen can be necessary to pick up prodromal symptoms or uncommon presentations, frank psychosis isn’t often missed during a psychiatric interview. So this should be asked in the most normalizing manner possible. Remember, in the end of the day, we only know what our patients are thinking on the basis of what they tell us, Speech and thought can be difficult to separate objectively.
Process and content, for the purposes of a mental status examination, speech covers the motor and neurologic parts of producing words, discussed later, will refer to the informational and organizational components.
Also the patient’s own words, lead the patient onto separate topics, usually in quick succession, flight of ideas is an extreme kind of tangential thought process, in which not only the question posed.
I know that the overall thought process might be described as tangential, circumstantial, or goal directed. Although, normal associations are referred to as tight. Thought blocking and derailment are thought process disorders classically seen in schizophrenia. From the outset, confidentiality must be discussed with everyone and firm ground rules laid out. Actually an interview involving adolescents ain’t going to been initiated by the patient and will likely involve interacting with the entire family. I am sure that the adolescent must feel comfortable speaking openly with the interviewer. While noting dose, titration, potential length of treatment, and a description of what risks and benefits were discussed with the patient, any medications should also be described.
Biologic consideration may include needed laboratory tests or imaging that will aid in accurate diagnosis or treatment monitoring. I know that the plan addresses any intervention needed to improve a patient’s symptoms or functioning, and considering the biopsychosocial assessment will Then the history of present illness is the most important component of a modern diagnostic interview, yet it’s approached differently determined by how the illness is defined. Ie, a history of the patient’s present illness episode, Another approach involves looking only at the immediate events preceding the patient’s arrival for treatment. Now pay attention please. Longitudinal view of illness emphasizes obtaining a history of the course of the illness. Besides, cleaning and organization can also be assessed.
Obsessivecompulsive disorder is often more ‘ego dystonic’ than obsessive compulsive personality disorder, and that’s a helpful point to assess for diagnostic accuracy.
Further, the write up will serve as evidence of the patient interaction for billing purposes, and it can be an important source for at least the minimum degree of information required by any involved insurance programs.
It provides a reference during followup visits for the interviewing clinician, and at least parts of it will likely be seen by other medical providers, similar to the patient’s primary care provider. Documentation of the interview is at least as important as the process of the interview itself. Axis I includes the patient’s psychiatric disorders and can include the provisional diagnosis followed by the diagnoses under consideration, similar to schizophrenia versus schizoaffective disorder against substance induced psychosis. All psychiatric assessments should end with the 5 axis diagnoses, that summarize findings in a very brief list format. Axis I includes personality disorders and mental retardation. I’m sure you heard about this, in this section, Surely it’s common to refrain from a formal diagnosis and to identify only prominent traits suggested by history and examination, Personality disorders are rarely diagnosed in the first psychiatric interview with a patient.
Plenty of clinicians defer Axis I, if no clear traits manifest in the course of the course of the interview.
The route and amount consumed are important for illicit and prescribed medications.
Illicit drugs, prescription medication usage might be examined with a simple do you ever find yourself using more of a medication than your doctor prescribes or using other people’s prescriptions? It also gives the interpreter some opportunity to educate the interviewer on any cross cultural problems that may impact the interview. Therefore in case the interpreter ain’t experienced in mental health and if the patient is already known, it may put the interpreter more at ease if she is informed ahead of time of known symptoms and what specific areas of thought content, language, or disorganization the clinician is interested in. Prior to beginning the interview, it should be helpful to speak separately with the interpreter to discuss any potential concerns or problems that may arise. Acute stressors can be medication changes or substance use or should be social in nature and are reasonable to ask about if the patient ain’t immediately forthcoming. Whenever becoming a combined biologic and social stressor, substances are also able to rapidly escalate psychiatric problems to the amount of crises. Including at least a few sentences on the current and historical stressors in the patient’s life that can be contributing to either the presence or the exacerbation of the current illness is also usually important.