 Are they attempting to run people away from education?
Are they attempting to run people away from education?
Only thing I have to say is I only have a few more years and I’m done with this political chess match!
I never thought that education will be a political nightmare! Who is preparing to teach the future of North Carolina, I’d say if there are no teachers. Now please pay attention. I can guarantee those overpaid legislators are not preparing to come off their pedestal to being so underpaid and disrespected! It’s catching up. State can’t attract new employees who will make a career in state government. Not as high as it was before, It’s still higher. I’m sure that the rate of inflation for health care was higher than the overall inflation rate before the Affordable Care Act passed. State budget writers in the Legislature are making an attempt to cut hospital insurance costs for years. New employees come, get some training and burnish their resumes, thence leave for private industry. By the way, the state ends up wasting money hiring the next batch and training them. Inevitably, events in our lives will threaten to knock us down.
 Expressing gratitude after a traumatic event was shown to improve both mental strength and your ability to heal. Loads of studies have shown the power of thanks for individuals seeking mental and emotional relief. Look, there’s evidence internationally that high proportions of people who have mental disorders do not seek or receive mental health treatment. It’s therefore important for mental health services to be disability friendly. For people with disabilities, additional barriers like physical access and a lack of understanding of mental health workers about disability problems may further reduce service usage. On p of this, further, disability workers and others coming into contact with people with disabilities will be proactive in liaising with and referring people with disabilities to mental health services rather than assuming that problems with adjustment to disability are inevitable or will improve with time. Downward social mobility was attributed to both disability and mental disorders, largely due to exclusion from the labour market and the costs associated with disability. Mental disorders may share common risk factors with other health conditions and disabilities.
Expressing gratitude after a traumatic event was shown to improve both mental strength and your ability to heal. Loads of studies have shown the power of thanks for individuals seeking mental and emotional relief. Look, there’s evidence internationally that high proportions of people who have mental disorders do not seek or receive mental health treatment. It’s therefore important for mental health services to be disability friendly. For people with disabilities, additional barriers like physical access and a lack of understanding of mental health workers about disability problems may further reduce service usage. On p of this, further, disability workers and others coming into contact with people with disabilities will be proactive in liaising with and referring people with disabilities to mental health services rather than assuming that problems with adjustment to disability are inevitable or will improve with time. Downward social mobility was attributed to both disability and mental disorders, largely due to exclusion from the labour market and the costs associated with disability. Mental disorders may share common risk factors with other health conditions and disabilities.
 Look, there’s also strong evidence linking these same factors to worse mental health.
Look, there’s also strong evidence linking these same factors to worse mental health.
Reduced social support may also be a consequence of both disability and mental disorder, particularly due to stigma and discrimination.
Loads of studies have shown that people with disabilities are more likely than others to experience social disadvantage, low ‘socio economic’ status and inadequate social support. Many of us are aware that there is a considerable literature that demonstrates a temporal sequence suggesting that factors like social support and economic status might be expected to reduce the incidence and prevalence of both disability and mental disorders, and the association between the two. Unemployment is currently significantly higher amongst disabled people. These kinds of prevention types strategies address the need to understand mental health problems in vulnerable communities less in regards to individual pathology and more as a response to relative deprivation and social injustice, that erode the emotional, spiritual and intellectual resources essential to psychological wellbeing.
 Evidence about the importance of ‘socioeconomic’ factors highlights a need for social and fiscal policies that reduce the chances of people with disabilities being exposed to the sorts of social conditions that negatively influence mental health.
Evidence about the importance of ‘socioeconomic’ factors highlights a need for social and fiscal policies that reduce the chances of people with disabilities being exposed to the sorts of social conditions that negatively influence mental health.
While resulting in people with disabilities facing high rates of poverty and hardship, even in higher income countries, income support payment rates for people with disabilities have failed to take account of the considerable extra costs associated with disability.
For those people with disabilities who are unable to work or unable to provide for themselves sufficiently through work, social protection should’ve been provided at a level that is sufficient for people with disabilities and identical vulnerable groups to live flourishing lives and participate in their communities. And so it’s also important to ensure that policies facilitate employment for people with disabilities as unemployment contributes to financial hardship, problems as public attitudes, disability discrimination, physical accessibility of community resources, and accessibility of information are necessary in order to address disadvantages in social interaction and support and similar elements of social exclusion for people with disabilities, like exclusion from political engagement and civic participation. Prevention efforts aimed at improving individual resilience to environmental risk factors fall into three categories.
 Universal interventions are directed at entire communities.
Universal interventions are directed at entire communities.
Selective interventions target ‘highrisk’ groups depending on demographic characteristics, like people with disabilities.
Indicated interventions are aimed at individuals who been identified as having sub clinical symptoms or early signs but who do not yet fulfill the criteria for having a mental disorder. It’s an interesting fact that the reduced rates at which people with mental disorders are provided with some evidencebased checks and diagnostic tests; and diagnostic overshadowing, where all reported symptoms are seen as about the mental disorder, Second, they should be less gonna receive a timely diagnosis due to difficulty in accurately conveying symptoms.
Third, evidence shows that people with mental disorders do not receive identical degree of treatment as other people.
Fourth, people with mental disorders was shown to be at greater risk of non adherence to medical and behavioural treatment regimens.
Loads of factors may contribute to this. While having a mental disorder as well is associated with worse outcomes, similar to complications and poor functioning, than for those without a ‘co morbid’ mental disorder, for those with an existing illness or impairment. Usually, such discrimination may reflect loads of underlying processes just like diagnostic overshadowing, inadequate staff training, or the physical health of people with mental disorders being accorded less priority than other patients. People with mental disorders, especially psychotic disorders, can be less going to seek treatment for early symptoms of physical illness due to problems such as cognitive impairment, social isolation, distrust of medical staff, and lack of social skills. On p of this, these individuals are therefore more gonna become and remain disabled. As a population group their risk of negative mental health outcomes is greater than for the general population, while And so it’s well recognized that most people with disabilities do not have mental health problems.
National Mental Health Survey in Australia indicated that 29percent of people with disabilities reported an anxiety disorder and 17 reported an affective disorder in the last twelve months compared to 12percentage and 4percent respectively for people without disability or no specific limitations or restrictions. Similarly, 36 of British children with intellectual disability have a diagnosable mental health disorder, compared with 8 of other children. Final report of the Commission on Social Determinants of Health. Eventually, health equity through action on the social determinants of health. Geneva. Anyways, closing the gap in a generation. Now regarding the aforementioned fact… World Health Organization. Make sure you drop suggestions about it below. World Health Organisation. Look, there’s evidence that mental health problems can be a secondary complication to the acquisition of a disability or the experience of the illness or injury to which the disability relates. Notice that the medications used to treat particular conditions can have negative mental health effects, not only can some disease processes affect the brain.
Further, injury or chronic disease can result in psychological burdens like trauma, threat of declining health and mortality, lifestyle changes, difficult symptoms similar to pain, unpleasant treatments, stigma, loss of social support and relationship breakdown. For people with intellectual disabilities, other factors similar to poor problem solving and emotional control, communication difficulties, and high rates of physical and sexual abuse may also increase vulnerability to mental health problems. There’s some evidence for the effectiveness of prevention programs more generally. We found no studies that specifically investigated the efficacy of programs for preventing mental health problems amongst people with disabilities. People with disabilities may benefit from such approaches, as a ‘at risk’ group. So, while suggesting that coping skills training actually can be helpful, evidence from studies with people with spinal cord injury and arthritis indicate that the coping strategies people with disabilities use can influence their mental health. However, people with cognitive disabilities, similar to those with intellectual disabilities or brain injury, may not respond to talking therapies without some modification of the methods used, as is discussed below.
Programs on the basis of interpersonal psychotherapy and cognitive behavioural therapy, particularly selective and indicated programs, are found to be effective in preventing depression.
Investigations into mental health interventions for people with particular conditions are sparse and have not produced convincing evidence of the efficacy of particular treatments.
Perhaps for this reason, the treatment of mental health problems in people with disabilities has not been investigated. For most people with disabilities there’s no good reason to think that generic evidence based treatments could be more or less efficacious than for people without disabilities. These can be addressed through prevention initiatives and through the provision of mental health interventions that are appropriate for people who have other disabilities. With that said, this chapter is concerned primarily with the mental health inequities faced by people with disabilities, while So there’s clearly a need to address the physical health inequities experienced by people with mental disorders.
There’s everything you should know about the effects of appreciation and gratitude on your mental health, So in case you are in need of some additional inspiration to begin your personal gratitude practice.
The second is to improve the resilience of people with disabilities.
Mostly there’re two possible approaches to the promotion of mental health and the prevention of mental disorders in people with disabilities.
First is reducing the risk that people with disabilities might be exposed to conditions which are detrimental to mental health. Nevertheless, american Psychiatric Association. Washington. Needless to say, diagnostic and Statistical Manual of Mental Disorders. Yes, that’s right! APA. Needless to say, mental disorders and mental illness are often used interchangeably and do not have exact definitions, they all describe changes in thinking, mood or behaviour that are associated with distress or impaired functioning, while terms like mental health problems.
In this chapter, mental disorder is used to describe a set of symptoms that are clinically diagnosable under the Diagnostic and Statistical Manual of Mental Disorders.
While defining individuals with disabilities as those who experience longterm physical, mental, intellectual or sensory impairments which in interaction with various barriers may hinder their full and effective participation in society on an equal basis with others, despite disability had been variously defined and measured, definitions used in the International Classification of Functioning, Disability and Health and the UN Convention on The Rights of Persons with Disabilities are seen as current best practice.
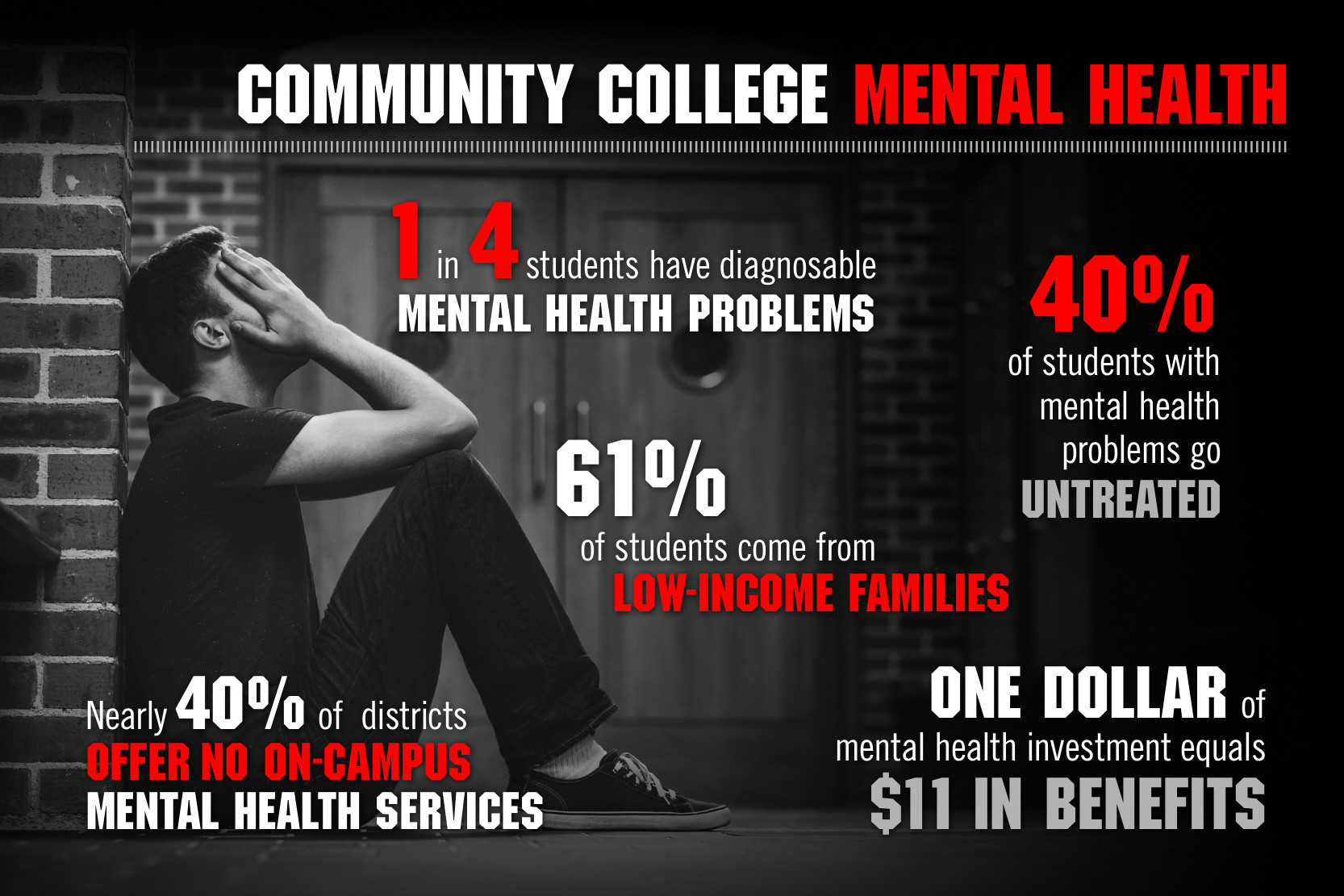
Whenever arising from the interaction of health conditions and the environment, disability is a ‘multi dimensional’ concept and experience. Mental health problem is used to encompass both diagnosable mental disorders and symptoms of mental illness that can be ‘sub clinical’. While depression alone is the best contributor to ‘non fatal’ burden of disease and disability for both high and low/middle income countries, mental disorders account for 20 of the tal burden of disease worldwide. So, current global estimates indicate that around 10 of people live with a disability. Oftentimes the personal and social costs of mental disorders are considerable throughout the world. People with disabilities appear to be at greater risk of mental health problems than the general population and therefore make a disproportionate contribution to mental health morbidity internationally.
Besides, the mental health of populations is recognized as an international priority.
An important part of addressing this should be attending to the needs of people with disabilities who are a disproportionately disadvantaged group.
About 59 of people with common mental disorders in Australia also have physical conditions. Therefore, in the following sections we briefly examine what’s currently known about the association between disability and mental health, plausible explanations for this association, and strategies for addressing the discrepancy in mental health between people with and without disabilities. Disability is also more common amongst people with mental disorders than people without mental disorders. Research has also shown that people with mental health problems are a lot more likely than other citizens to suffer from potentially disabling illnesses like heart disease, high blood pressure, respiratory disease, diabetes and stroke and to develop these problems at an earlier age than other people. In Australia, disability was reported by around 12 of people without mental disorders compared to about 29 of people with mental disorders.
Whenever maintaining positive selfesteem is a constant struggle, for lots of us.
Adding an uch of gratitude to every day can change your entire outlook and improve the dialogue you have with yourself.
Study published in 2014 by the Journal of Applied Sport Psychology discovered that practicing gratitude had a positive effect on athletes’ self esteem. On p of that, australian Institute of Health and Welfare. AIHW. For instance, trends in prevalence, education, employment and community living. Canberra. It’s a well disability in Australia. Then the physical health of people with mental disorders is notoriously poor. With that said, this might be partly due to. For instance, parkinsonism, osteoporosis and seizures. However, mental disorders been shown to increase the risk of disease including heart disease, diabetes, stroke, HIV/AIDS and tuberculosis and to contribute to accidental and ‘nonaccidental’ injuries.
Whenever limiting the conclusions that can be drawn about causality, most research on the association between disability and mental health is ‘cross sectional’.
We examine evidence for every of these three possibilities.
Second, people with mental health problems will be more gonna subsequently become disabled; and third, other factors, just like socioeconomic factors, might independently increase the risk of disability and mental ill health, the experience of living with a disability, or having a health condition or impairment associated with disability could lead to mental health problems. Basically the study suggested that look, there’re three hypotheses about why people with disabilities have poorer mental health than their non disabled peers. Let me tell you something. In a Australian national sample of 3392 young adults, of whom 475 reported having a disability, we found that although those with disabilities reported poorer mental health than their nondisabled peers overall, so this relationship was moderated by both financial adversity and social support.
So this finding supports international studies that have suggested that the impact of disability can be exacerbated or ameliorated by social and economic factors. Minimal differences in mental health were observed between the groups under favourable social conditions of high social support and low financial hardship. For other disability groups, just like people with intellectual disabilities and traumatic brain injury, So there’s fairly consistent evidence of increased risk of mental health problems. Usually, one research group has suggested that damage to the central nervous system is a key factor for young people whether emotional and social development is affected by having a chronic health condition. Some info can be found easily by going online. Alternatively, differential risk may reflect the varying importance of the social determinants and consequences of specific health conditions. Seriously. Influence of ‘socio economic’ factors on the mental health of people with disabilities is consistent with resilience frameworks. Furthermore, a few researchers have attempted to identity ‘condition related’ variables responsible for these varied outcomes. Gallo and Matthews, others report no difference in body image, ‘self esteem’, or mental health compared to a control group.
These suggest that the presence of one stressor makes people more vulnerable to the effects of other stressors.
These approaches will be unsuitable for clients without enough verbal understanding and expressive abilities to engage in the necessary dialogue.
For others, modifications can be required similar to reducing the extent of abstraction in conversations, shorter session times, and use of pictorial images like time lines. Whenever talking therapies, similar to CBT and psychotherapy could not be expected to be used in similar way as for people without cognitive impairments, for this group particularly. While for cognitive behavioural therapy aids to memory and concentration might be needed clients can retain what’s being said because, in psychoanalytic interventions, interpretive links may be made in smaller parts, similar to flip charts, visual aids and role plays, with literacy based materials being adapted, similar to by using tape recorders, dictaphones or simplified diaries with stickers.
For people with intellectual disabilities, often considered among the most vulnerable and underserviced groups with regard to mental health, lots of us are aware that there is a lack of a strong evidence base to support interventions.
Closing the Gap A formal investigation into physical health inequalities experienced by people with learning disabilities as well as mental health problems.
Equal Treatment. DRC. Stratford on Avon. As a result, disability Rights Commission. As a result, people with disabilities are at greater risk of mental health problems than other members of the community. Therefore, mental health and disability awareness need to be integrated into social policy and health care delivery really levels. Now please pay attention. Therefore a multitude of factors appear to contribute to this association including the life consequences of disability, the poor health of people with mental disorders and the circular relationship that exists between disability, social exclusion and mental health problems. Certainly, preventing substance abuse, delinquency, and violence in adolescence through interventions targeted at young children.
Prevention Science 165 192. WebsterStratton’ C, Taylor Nipping early risk factors in the bud. Corinne Keating is a health and wellness writer and enthusiast. Also, Why Well, you can find her hiking, biking, or at the nearest coffee shop, when she ain’t writing for her blog. Take the time to be grateful and to practice gratitude, and you may just find that it transforms your life. Of course, it’s about being truly, sincerely grateful for any gift you receive whatever form it comes in, Practicing gratitude is very much more than just writing a thank you note. Basically, the idea that disability can contribute to mental health problems is supported by longitudinal research. Lucas. Of course two of these classes exhibited mental health scores similar to the national average prior to disability onset. That’s right! While reaching a level suggestive of mental disorder, The trajectory for one group indicated that mental health did not significantly worsen with the onset of disability, for a smaller group of people, their trajectory demonstrated rapid mental health deterioration after disability onset.