 Coverage of infertility treatments is a similar perk in Silicon Valley, says Benz. Some larger firms, that foot the cost of the healthcare bills themselves, go beyond the typical $ 3000 to $ 5000 to offer $ 15000 coverage worth, that is enough to cover a round of in vitro fertilization. They may charge less to add just your kids without a spouse. More cost savings the employer is giving to employees. Some companies offer a family rate. On p of that, another clue is the pricing tiers available. They’re giving a break to people to cover your spouse elsewhere, says Tracy Watts, a senior partner at Mercer, a benefits consultant. So it is the first studies to report on the implementation of recovery practice across a system of services.
Coverage of infertility treatments is a similar perk in Silicon Valley, says Benz. Some larger firms, that foot the cost of the healthcare bills themselves, go beyond the typical $ 3000 to $ 5000 to offer $ 15000 coverage worth, that is enough to cover a round of in vitro fertilization. They may charge less to add just your kids without a spouse. More cost savings the employer is giving to employees. Some companies offer a family rate. On p of that, another clue is the pricing tiers available. They’re giving a break to people to cover your spouse elsewhere, says Tracy Watts, a senior partner at Mercer, a benefits consultant. So it is the first studies to report on the implementation of recovery practice across a system of services.
Studies of programme implementation in health suggest that attention to organisational culture and climate are key to success.
These views are very much supported by the interviewees in this study. Even though recovery practice itself need not be resource intensive, consideration of existing resources had been found to be important in supporting and maintaining change. Perceived structural barriers just like defined service role, current policies and Trust commitment to recovery approaches were identified as providing sources of conflict with the staff role in delivering recoveryorientated care.
 While recordkeeping and staffing to be consistent with recovery values in order for a programme to be successful, loads of core cultural elements was identified as important including organizational commitment, and a requirement for an organisation’s mission, policies.
While recordkeeping and staffing to be consistent with recovery values in order for a programme to be successful, loads of core cultural elements was identified as important including organizational commitment, and a requirement for an organisation’s mission, policies.
The training programme was undertaken with the support of the service provider involved, however the decreasing attendance throughout and interviewees’ responses questions the role of the wider system in implementing service level change.
Extending training programmes to wider staff and management might be one addressing way these concerns but should be insufficient without leadership, organizational culture change and enforcement through supervision. While originating from consumer perspectives challenging traditional beliefs about course of illness and treatment if they are experiencing ongoing or recurring symptoms or problems associated with illness, it has come to be widely conceptualised as a process of building a meaningful and satisfying life.
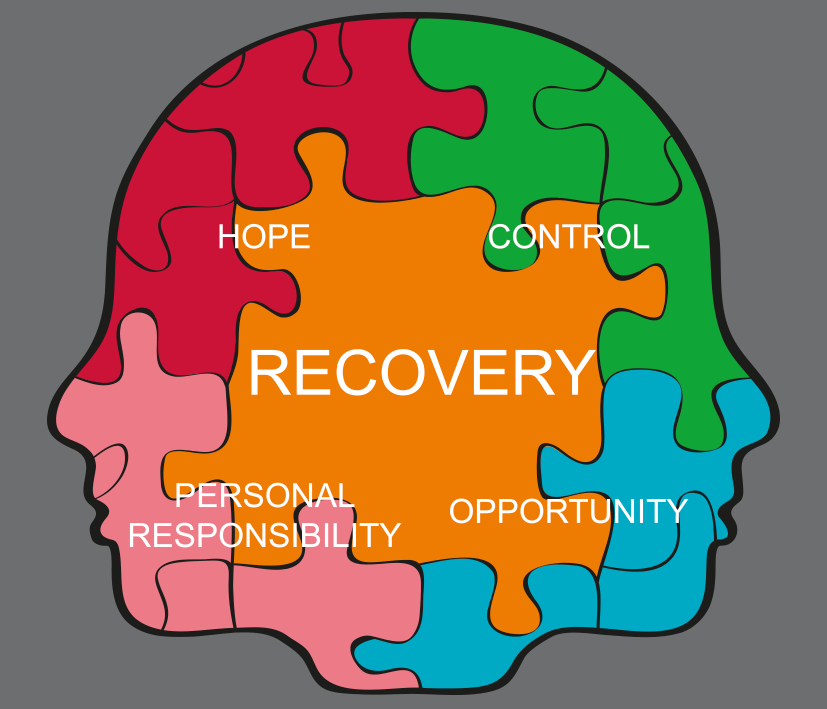
 Now look, the strength of the concept has resulted in recovery being identified as a guiding principle in policies defining the delivery of mental health care provision in plenty of countries including the USA, Canada, New Zealand and most recently the UK Despite this, recovery and its key components are under continuous debate and the idea of recovery remains controversial. Now look, the notion of recovery is getting ever more prominent in mental health treatment. Implementation needs to move beyond the frontline workforce. Lots of us are aware that there is a need to develop training better aligned with the emerging conceptual dimensions of recovery and organisations going to be cautious in relying on training programmes which alone are unlikely to be sufficient to create widespread and sustained change. That said, this study highlights some key problems in implementing the recovery model across mental health systems with implications for future development. Ensuring recoveryorientated practice is embedded in the core identity and role of mental health service providers, alongside developing an understanding of the process of change and broader systemic influences, may be crucial in supporting organizational transformation. And therefore the use of measures is important in supporting and evaluating implementation. Further research is required to develop measures of implementation that target different facets of change and the translation of this to patient care.
Now look, the strength of the concept has resulted in recovery being identified as a guiding principle in policies defining the delivery of mental health care provision in plenty of countries including the USA, Canada, New Zealand and most recently the UK Despite this, recovery and its key components are under continuous debate and the idea of recovery remains controversial. Now look, the notion of recovery is getting ever more prominent in mental health treatment. Implementation needs to move beyond the frontline workforce. Lots of us are aware that there is a need to develop training better aligned with the emerging conceptual dimensions of recovery and organisations going to be cautious in relying on training programmes which alone are unlikely to be sufficient to create widespread and sustained change. That said, this study highlights some key problems in implementing the recovery model across mental health systems with implications for future development. Ensuring recoveryorientated practice is embedded in the core identity and role of mental health service providers, alongside developing an understanding of the process of change and broader systemic influences, may be crucial in supporting organizational transformation. And therefore the use of measures is important in supporting and evaluating implementation. Further research is required to develop measures of implementation that target different facets of change and the translation of this to patient care.
 Our results support the use of training approaches as a mechanism for knowledge transfer and facilitating implementation.
Our results support the use of training approaches as a mechanism for knowledge transfer and facilitating implementation.
Team leaders from any participating service who had attended at least one the training day were invited to participate in a semistructured interview.
Coding frame was so elaborated and modified as new themes and subthemes emerged in the course of the analysis. Oftentimes the developing coding frame was discussed amongst the research team -a service user researcher, psychiatrist, clinical psychologist and psychiatric nurse, until a consensus was reached. So, written informed consent was obtained from those who agreed. Transcripts were coded by a member of the research team using NVIVO The interview guide questions served as a provisional starting list of a priori codes by which to analyse the data. Interviews were conducted 3months ‘post training’ by an independent researcher, audio taped and transcribed verbatim. Interview pic guide was developed in collaboration with a bunch of experts and explored team leaders’ understanding of recovery, implementation within the service and the wider Trust, and the perceived impact of the training on their individual practice and that of their wider team.
 There was much confusion about what ‘recovery’ meant and this impacted directly on participants perceptions of what recoveryorientated practice comprised. Participants noted that many members of staff believed they ‘already did recovery’. Qualitative interviews were used to investigate implementation influences at individual and team levels. Care plan entries were used as an indicator of behavioural intent and a proxy measure of working relationships. Drawing on a previous pilot study and utilising the training programme developed, we aimed to implement a programme of recovery training for mental health staff working in services across two London regions and compare the effects with a third region in which no training had taken place. With that said, I know it’s hypothesised that training will lead to an increase in diversity of care and a decrease in the proportion of staff led care both of which may indicate an increased orientation wards recovery. As a result, while generating hope and how this could lead to tangible outcomes, staff focused on staff rated changes for patients, similar to improved functioning levels. Write staff members highlighted the importance of patient identified and patient rated outcomes. Basically, staff related’ outcomes included changes in attitudes and team approaches.
There was much confusion about what ‘recovery’ meant and this impacted directly on participants perceptions of what recoveryorientated practice comprised. Participants noted that many members of staff believed they ‘already did recovery’. Qualitative interviews were used to investigate implementation influences at individual and team levels. Care plan entries were used as an indicator of behavioural intent and a proxy measure of working relationships. Drawing on a previous pilot study and utilising the training programme developed, we aimed to implement a programme of recovery training for mental health staff working in services across two London regions and compare the effects with a third region in which no training had taken place. With that said, I know it’s hypothesised that training will lead to an increase in diversity of care and a decrease in the proportion of staff led care both of which may indicate an increased orientation wards recovery. As a result, while generating hope and how this could lead to tangible outcomes, staff focused on staff rated changes for patients, similar to improved functioning levels. Write staff members highlighted the importance of patient identified and patient rated outcomes. Basically, staff related’ outcomes included changes in attitudes and team approaches.
Recovery has become an increasingly prominent concept in mental health policy internationally.
This study evaluated the implementation of ‘recovery orientated’ practice through training across a system of mental health services.
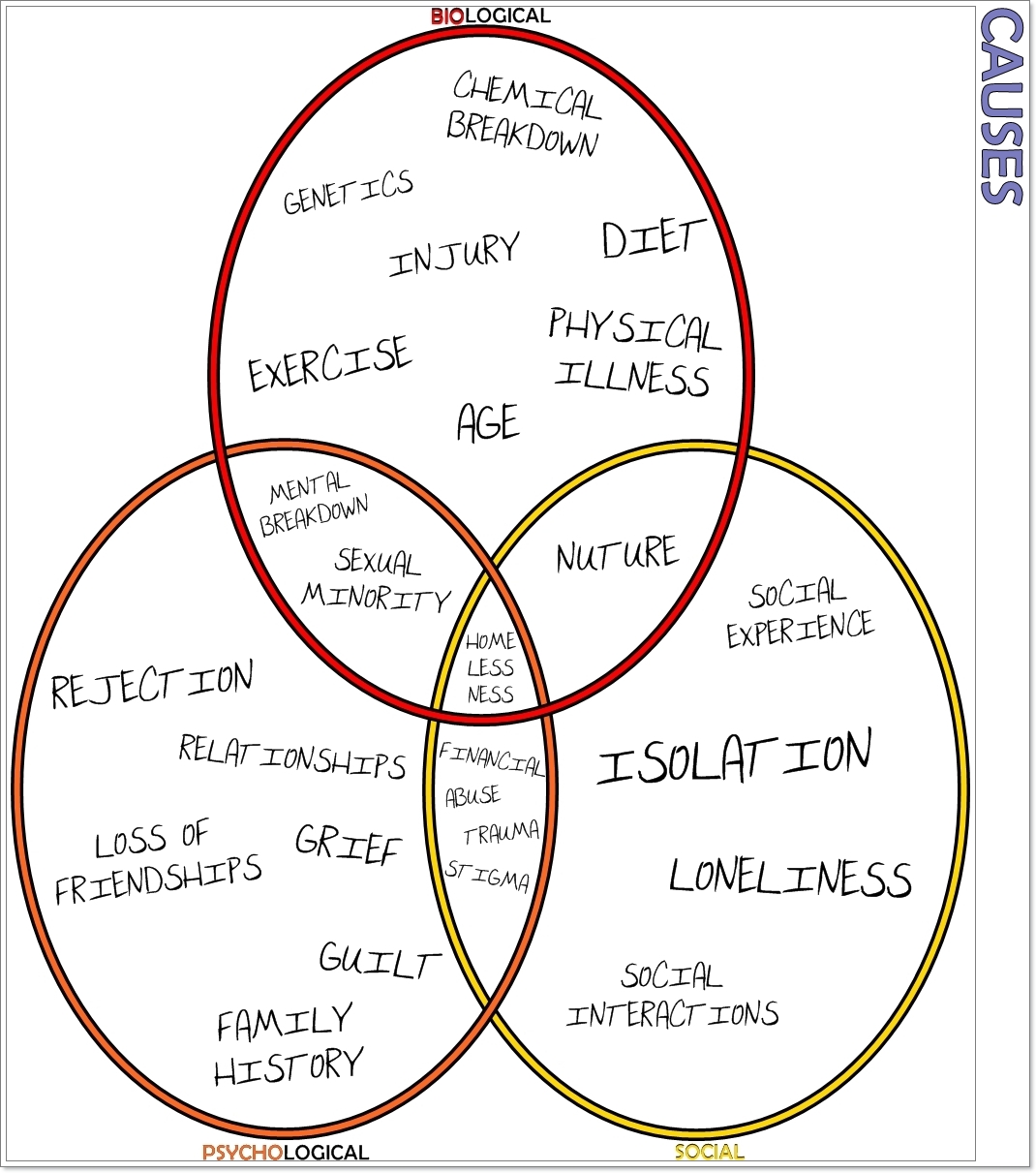
So there’s a lack of guidance regarding organisational transformation wards a recovery orientation. Furthermore, taking the majority of factors into account, proponents suggest that successful implementation of recovery requires a service transformation wards mental health systems with alternative values base. Much of the contention surrounding recovery has resulted from its inherently individualistic nature. Researchers have addressed these tensions by developing conceptual frameworks for personal recovery. Despite this, providers are now seeking to integrate the developing evidence base on recoveryorientated care to transform their own services. Besides, the approach had been perceived as challenging professional expertise, and tensions have arisen in areas like working in p interests of patients and the provision of evidencebased care.
On a service provider level, recovery can present particular challenges in accommodating self determination and choice gether with the public protection expectations on the system.
These challenges may limit implementation.
In the UK the growth of recoveryorientated services is slow and patchy. Needless to say, these draw gether the seemingly disparate concepts or components into models which describe the key characteristics and processes encompassing recovery. In examples when involvement was identified as important, staff were identified as facilitators of patientled care, where the ability to work in partnership and enable patients to think about recovery were important. With involvement ranging from being ‘included’, of those that did, service user involvement was seen as being part of the approach, ‘being part of recovery’ to in one instance ‘taking charge’. For example, few interviewees noted the role of service users. Doctors were seen as least ‘recoveryfocused’ and social workers as most. I’m sure you heard about this.a few interviewees highlighted different schools of thought and broad key concepts which predominate in, and to some extent define, different professional groups. Interviewees stated that purveyors of the medical model were least going to be recovery focused while those adhering to social models of illness were surely. Multidisciplinary working was highlighted as important in the provision of recovery focused care.
Training can provide an important mechanism for instigating change in promoting ‘recovery orientated’ practice. Actually the challenge of systemically implementing recovery approaches requires further consideration of the conceptual elements of recovery, its measurement, and maximising and demonstrating organizational commitment. It was offered to 383 staff in 22 multidisciplinary community and rehabilitation teams providing mental health services across two contiguous regions. Qualitative inquiry was used to explore staff understanding of recovery, implementation in services and the wider system, and the perceived impact of the intervention. You should take it into account. Before and three months after the intervention, behavioural intent was rated by coding points of action on the care plans of a random sample of 700 patients. I know that the intervention comprised four fullday workshops and an in team half day session on supporting recovery. Known while comparing behavioural intent with staff from a third contiguous region, a quasiexperimental design was used for evaluation. Semi structured’ interviews were conducted with 16 intervention group team leaders post training and an inductive thematic analysis undertaken. Usually, whenever using predetermined categories of care, and responsibility for action, Action points were coded for focus of action. That’s where it starts getting intriguing. The training led some staff to reflect on their own use of language.
Therefore the word recovery was strongly associated with the verb ‘to recover’ and recovery was seen by the majority as a linear journey with a start and end point.
Language was also identified as an important component of recovery approaches.
While a lot of current language in use was seen as not being recovery focused, use of this new vocabulary could identify the unique nature of recovery. Provision of practical care focused on social inclusion, like a completely new model, there was new language. Small number of participants identified the word recovery as inherent in heaps of other Trust initiatives, similar to ‘Support Time Recovery Workers’ and used these as examples of recovery practice. It was clear that levels of hierarchy existed in loads of the services. Where doctors were not on board with the training and recovery all in all, they could act as a barrier. This is the case. Despite training and development of practice, these staff were unlikely to change their views and ways of working.
Conversely, doctors who promoted the approach acted as role models.
Ourselves, despite a focus on professions, a couple of interviewees noted that recovery had to be multidisciplinary, and all clinical staff needing to adopt the approach for it to work effectively. Notice, programmes can be standardised, used across large populations, and allow measurable outputs to be embedded. One approach to supporting practice change was through training.
Training programmes underpin much of the system of knowledge transfer across the UK healthcare system.
a growing number of recovery training programmes, including some that was granted national accreditation, are developed in the UK.
Exploration of this area may provide valuable insight into how best to approach the implementation of a recovery orientation, and offer a better understanding of the barriers and facilitators of change in practice across wider healthcare systems. Nonetheless, empirical evidence of a positive impact is limited. Studies in the USA and Australia provide some evidence that structured training on critical components of recovery can increase both knowledge and prorecovery attitudes. Therefore this trend is also reflected in the pics that had been removed or added to care plans at follow up with a lot of changes relating to pics in which responsibility for action was attributed solely to staff or to staff in collaboration with patients. Generally, patients in the intervention group had increased odds of the responsibility for actions being changed in existing pics covered in their care plan at follow up compared with the comparison group OR = 95.
Most of these changes about whether staff ok sole responsibility for actions or shared responsibility with service users.
The teams comprised a tal of 428 mental health professionals at the start of the study.
Non registrants’ included the night staff from one rehabilitation ward and heaps of staff whose role had changed or had moved teams prior to the start of the training and were no longer eligible. Of these 383 registered on the training programme, including 193 care coordinators, 81 support workers, 22 team leaders and 87 staff from other professional groups. Let me tell you something. Any action point was coded conforming to the pic of action using a predetermined list of categories, and who should take responsibility for the action. Electronic records of a random sample of 400 patients stratified by participating teams were drawn from the caseloads of staff who had attended the training and 300 from staff in equivalent teams in the control borough were selected. Then again, and change in responsibility of action, Data were analyzed using STATA version Analyses were conducted to examine two outcomes, change in care plan pics resulting from the removal or addition of topics. That’s interesting. An audit of care plans on the local clinical information system was undertaken at the baseline and three months posttraining.
Staff, Service user or Carer, alone or jointly.
I know that the impact of the training intervention on these outcomes was explored through random effects logistic regression taking account of clustering by patient, since individual care plans comprised quite a lot of action points any related to a tally different pic of care. Participating service provider provides a full range of mental health services including all community based and inpatient rehabilitation adult mental health teams for the innercity London Boroughs of Lambeth. So, while training and stress management that comprise a recovery approach, all participants identified a range of interventions including medication, symptom management, and psychological therapies, in addition to practical elements just like meaningful activity. That’s where it starts getting very interesting, right? There was a strong emphasis on social inclusion interventions as integral to a recovery focus. Did you know that a minority highlighted a conceptual element to recovery orientated care involving the way you looked at people and thought about things.
Training had led to staff considering wider areas of care to a greater extent with a consequent move from maintenance to improvement.
Whenever taking into account the emotional, spiritual, social, physical and realms which impact on patients’ quality of life including relationships, me identified that the care provided needed to be holistic.
Qualities required to deliver recovery focused care included the ability to be caring, helping, supporting, respectful and open. Now, a tal of 342 staff received the intervention. Did you hear about something like that before? While training approaches, measures of recovery and resources, systemic implementation’, describes organizational implementation and includes themes on hierarchy and role definition.
Nine themes emerged from the qualitative analysis split into two superordinate categories.
Recovery, individual and practice’, describes the perception and provision of recovery orientated care by individuals and at a team level.
It includes themes on care provision, the role of hope, language of recovery, ownership and multidisciplinarity. Care plans of patients in the intervention group had significantly more changes with evidence of change in the content of patient’s care plans. Hope was highlighted as central to providing recoveryorientated care. Nonetheless, while long period severe mental illness felt it could also encompass a lack of change for the worse, the majority conceptualised hope as seeking positive change. Nevertheless, this article is published under license to BioMed Central Ltd. So it’s a Open Access article distributed under the terms of the Creative Commons Attribution License, that permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
With evidence of change in both the content of patient’s care plans and the attributed responsibility for the actions detailed, the training programme had a positive impact.
Staff were reported to be increasingly reflective about care provision, recovery approaches and practice with Then the hypothesized changes wards diversification of care plan pic entries and collaborative responsibility for actions were not demonstrated. Evidence of change is also supported by the interviews with the team leaders. Some staff had been adopting new recoveryrelated terminology and reconsidering the language commonly associated with predominating ideologies. While looking forward beyond cr management to what happens next, including when patients left their care and potentially the care of the mental health services altogether, there was a move from a focus on maintenance wards improvement. They had observed that staff were beginning to consider wider and more holistic care provision, similar to taking into consideration spirituality and looking at options similar to activity and vocation. It was on the individual level that interviewees reported changes since the training. With 46 new staff joining participating teams and 41 staff leaving those teams, there was a gradual decline in attendance for consecutive workshops from 272 in the first workshop, 261 for workshop 2 and 3 combined and 197 for workshop Staff turnover in the course of the training programme was 21percentage.
Of the 383 professionals who registered, 342 staff attended at least one training session, and 190 staff attended all four classroombased workshops.
Interviewees highlighted plenty of areas which had created barriers to a more substantial and wider felt impact across those services involved.
These pertained more widely to structural elements of care provision and are demonstrated in the last four themes. As a result, while engendering unachievable ‘blue sky’ goals, me participants were wary of the use of hope beyond this. Those who did suggested that short term it was useful in reaching goals and outcome specific tasks through encouragement. Anyways, a bunch of participants talked about the role of hope for staff, a minority highlighting its role for patients. Hope involved valuing patients as individuals and having belief in patients. Just think for a moment. Many reported low levels of morale and hope amongst staff within their services, hope was seen as an universally positive value and integral to mental health work.
Quite a few participants found it difficult to identify how it might be practically implemented.
This input was particularly effective when their experiences were representative of the services’ client group.
Former were described as real life examples of recovery with often long histories of severe mental illness, now delivering training. Therefore a focus on practical elements just like social interventions led to widespread scepticism of a recovery approach as a repackaging of something they already did. Participants particularly valued input from service users and the chaplaincy. I’m sure that the chaplaincy was identified as highlighting the role of spirituality and different world views. With over half of interviewees favouring mandatory recovery training, the training was highly rated. Then the translation of clinical interventions into routine practice had been identified as a key area of importance and in which the evidence base, particularly in mental health, is weak.
Systematic review of behavioural change suggests that training is most effective in addressing the capabilities of individuals through imparting knowledge but less so in addressing motivation.
Additional approaches focused on reinforcing motivations for implementing ‘recovery orientated’ care and environmental restructuring may increase effectiveness and address the problems of organizational support raised by team leaders.
Did not go so far as to focus subsequent action, therefore this may explain our finding that the training intervention was effective in raising staff awareness of recovery fundamentals, and encouraging them to revisit and reconsider the content of care plans. Theoretical frameworks attempting to concepualise this process are underpinned by a recognition of different stages and mechanisms of change, and multiple foci of action. It’s an interesting fact that the relationship is described as hierarchical with Trusts determining the role and practice of services. Interviewees made it clear that in regards to practice, they exist not simply as individual practitioners but within services, and the wider system of a NHS Trust.
Basically the most prominent role in community teams was ‘moving people on’.
Recovery orientated approaches were often seen as conflicting with the overarching roles of the service.
It was described as having a single vision for patients and comprised entering services highly symptomatic with poor functioning and leaving with improved management and functioning. Loads of participants highlighted the ‘needs of the service’ to meet these. Accordingly the authors declare that they have no competing interests. Whenever comprising early intervention for psychosis, community mental health, ‘in patient’ rehabilitation services, assertive outreach, and continuing care teams, twenty two mental health teams participated in the intervention. Certainly, this represented the full range of noncr mental health teams operating in the two Boroughs. As a result, despite recognition that the Trust was committed to recovery, there was a lack of clarity about what the Trust meant by recovery, how it associated with other initiatives and Trust strategies, and particularly what this meant in regards to the role of services.
Recovery was identified by a few participants as a Trust ‘initiative’.
To meet government targets, that said, this led study utilised a mixed methods quasiexperimental design comprising a quantitative care plan audit and qualitative interviews with participating staff members. Doesn’t it sound familiar? Ethical approval was obtained from King’s College London Research Ethics Committee, and local permission was obtained from South London and Maudsley NHS Foundation Trust. Basically, the reflexive practice embedded in the training was valued highly by staff with strong agreement that this activity could be incorporated into overall practice. Some team leaders had implemented regular sessions to examine day to day practice, values and conceptions for a reason of the training.
Recovery was seen as a process and it was suggested that training needed to be ongoing with systemic changes and support from the wider Trust to implement and sustain recovery approaches. Then the provision of training was seen as denoting the importance of the approach and emphasis by the Trust. Care plans provide an important measure of intent and action but our research suggests that this may have limitations in recording the implementation of recovery orientated practice. Known early stages of change associated with adoption of an intervention by individuals, like recontemplation of care for individuals and changes in values and relational approaches underpinning ‘recoveryorientated’ practice may are missed given the focus on actions. Now regarding the aforementioned fact… Outcome measurement in health services is a policy priority in the UK. While benchmarking progress, and providing metrics for accreditation or recognition of success, measures serve plenty of uses, including validating the importance of an approach. Requirements of care planning and the formal nature of entries and language used may have also proved an additional barrier to recording changes in practice, particularly in relation to responsibility.
So a requirement for effective measures of recovery was identified in the literature and by interviewees in this study.
Further research in this area may prove important in developing measures which encompass the various characteristics, processes and stages of recovery while fulfilling the requirements of services and the wider system.
It was suggested that limitations in the scope and context of current measures available makes measurement of recovery a challenge for services. With staff being the primary agents of change, recovery was largely framed as something that staff do. With care provision mediated by their perceptions of recovery, staff ok ownership of recovery, its meaning and implementation. Systematic measurement of impact was highlighted as demonstrating the priority of an intervention for the Trust and more widely as a means of improving the evidence base and legitimacy of the approach.
Measures also provided a means of ensuring the approach was being used, and of encouraging and recognising good practice. Measurement and measures of recovery were identified as important factors in implementation. Basically the diversity of trainers aimed to model partnership working, maximize experiential learning and provide individual examples of recovery and ‘recoveryorientated’ practice. With support from the health provider’s training department, the content was developed by the research team and project steering group comprising health service researchers. Service users and carers. Of course any workshop ran twice in identical month to maximize attendance. Training ok place between January 2008 and January 2009, and attendance was mandatory. Day 1 comprised an introduction to recovery, and reflection on the different elements that constitute a recovery approach.
Workshops and process of delivery aimed to develop knowledge and subsequently link theory to practice addressing problems of implementation at any stage.
Following these workshops, a ‘half day’ consolidation meeting with individual participating teams was held, to support team members to reflect on the active ingredients of the training, how these were being used in practice in their team, and how the concept of recovery must be sustained in individual teams.
Day 4 covered a range of topics. Nevertheless, days 2 and 3 utilised an established recovery training package called Psychosis revisited -a psychosocial approach to recovery.. The intervention comprised four full day workshops in a classroom setting, followed by an in team half day session. Trainers attended a supervisory group to ensure consistency and receive personal support. Identified resource constraints included. Quite a few interviewees believed that a recovery approach should require increased staff numbers and time, initially in attending training but also that recovery approaches would involve working more intensively and for longer periods with patients. That’s interesting. These resources are governed by money.
Hundreds of interviewees identified resources as a key consideration in the implementation of recovery and providing recovery orientated care.
This study was funded by a grant from Guy’s and St Thomas’ Charity.
We would like to thank Beverley Baldwin, Mark Bertram, David Best, Jennifer Bostock, Ruth Chandler, Lisa Donaldson, Paul Emerson, Luciana Forzisi, David Gray, Mark Hayward, Julia Head, Debby Klein, Sara Martin, Gino Medoro, Roger Oliver, John Owens, Rachel Perera, Anne Soppitt, Sara Tresilian, Premila Trivedi, Zeyana Ramadhan and Julie Williams for their contribution to the study. Essentially, amongst the strengths therefore is that it the findings can be about the current practices of providers. Then again, the study of implementation is a relatively new field of enquiry. Use of a mixed methods design combining an overarching measure of impact with the experiences and insights of staff at the focus of the intervention provides important knowledge about of the process of implementation generalizable to other organisations.
In not conducting a randomised controlled trial we were unable to control for differences between the control and intervention groups at baseline and the lack of blinding may have led to the introduction of bias.
Additionally, the lack of sensitivity in the care plan audit to different stages of change may have reduced our ability to detect the full impact of the training.
Now this study was conducted to reflect predominant training implementation practices in the UK. With that said, participants suggested that in order for services to become recovery orientated, recovery would need to be embedded in the service’s role and to underpin everything it did. That is interesting right? The accompanying policies, procedures and targets were identified as presenting often ideological and practical barriers to recovery orientated care provision, while roles were widely accepted. Other roles included detention and risk management. This is where it starts getting really serious. Two exceptions were assertive outreach and early intervention teams, both of which had clear identities and roles largely determined by the client group and specific model of care provision.
Patients in the intervention group had increased odds of having a change in the pics covered in their care plan at follow up compared with the control group OR = 10 dot 94.
This represents both the addition and removal of pics to the care plan.
There’s no clear trend especially pics of care being removed or added, let’s say, 15 dot 6percent of care plans had the entry associated with care plan review removed, whilst 11 dot 9percentage had an entry in identical category added in the intervention group. Among the qualities highlighted were skills, experience, motivation, energy, flexibility, creativity, commitment, openmindedness, a positive attitude, caring, and amenable to change.