 What if you die after the 20 year Term life policy expires?
What if you die after the 20 year Term life policy expires?
Oh yes, and you can quit making investment contributions and not lose anything.
If you live until you’re 80, your heirs shall not receive any insurance money, however there’s absolutely no telling how much they will receive from your investment, with Term life. You will continue to make premium payments with a Whole life policy, however all that your heirs will get is the face value of the policy, if you live 40 more years until you are 80, Therefore in case you buy a 20 year Term life insurance policy when you are 40. Now after 20 years, the Term life policy has expired but who needs it. You are now out of debt and your home is fully paid for, if you was a prudent manager of your finances. Your spouse will have to be happy with only the huge earnings that your investments have yielded for you, if you die. Samesex sexual orientation Factors that may decrease the risk for suicide are also called protective factors.
And, after helping a friend, family member, or patient during a mental health cr, be aware of how you may was affected emotionally and seek the necessary support for yourself.
 These include. Whenever acting reckless or engaging in risky activities, you may have to be active and persistent in helping them to get the in the course of the initial treatment phase because of the potential for the possible emergence of suicidal ideation and behaviors during this time. Because of the relationship between low CSF serotonin levels and the emergence of aggression and impulsivity, the selective serotonin reuptake inhibitors been recommended for the treatment of depressive disorders when suicidal risk is present. I’m sure you heard about this. Staying within VHA clinical practice guidelines, That’s a fact, it’s indicated to prescribe anxiolytics, sedative/hypnotics, and shortacting antipsychotic medications up to or at the maximum indicated dosages to directly address agitation, irritability, psychic anxiety, insomnia, and acute psychosis, until such time as a behavioral health assessment can be made. Lots of information can be found easily online.a single two ‘evidencebased’ medications that was shown to lower suicidal behaviors are lithium and clozapine. I’m sure that the most common psychiatric symptoms associated with acute risk for suicidal behaviors include. Actually, these medications do not reach therapeutic levels immediately. By the way, the amount and medications type to address these clinical presentations needs to be carefully chosen and titrated when the individual is deemed to be under the influence of alcohol, illicit substances, and akin medication in prescribed or overdose amounts. Although depressive symptoms are often associated with risk for suicide, no antidepressant medication has yet to be shown to lower suicide risk in depressed patients.
These include. Whenever acting reckless or engaging in risky activities, you may have to be active and persistent in helping them to get the in the course of the initial treatment phase because of the potential for the possible emergence of suicidal ideation and behaviors during this time. Because of the relationship between low CSF serotonin levels and the emergence of aggression and impulsivity, the selective serotonin reuptake inhibitors been recommended for the treatment of depressive disorders when suicidal risk is present. I’m sure you heard about this. Staying within VHA clinical practice guidelines, That’s a fact, it’s indicated to prescribe anxiolytics, sedative/hypnotics, and shortacting antipsychotic medications up to or at the maximum indicated dosages to directly address agitation, irritability, psychic anxiety, insomnia, and acute psychosis, until such time as a behavioral health assessment can be made. Lots of information can be found easily online.a single two ‘evidencebased’ medications that was shown to lower suicidal behaviors are lithium and clozapine. I’m sure that the most common psychiatric symptoms associated with acute risk for suicidal behaviors include. Actually, these medications do not reach therapeutic levels immediately. By the way, the amount and medications type to address these clinical presentations needs to be carefully chosen and titrated when the individual is deemed to be under the influence of alcohol, illicit substances, and akin medication in prescribed or overdose amounts. Although depressive symptoms are often associated with risk for suicide, no antidepressant medication has yet to be shown to lower suicide risk in depressed patients.
Sedatives/hypnotics are recommended for symptoms of insomnia, and anxiolytics for the treatment of anxiety and agitation.
Practice Guidelines for the Assessment and Treatment of Patients with Suicidal Behaviors.
In. For instance. While dying or suicide The remaining list of warning signs must alert the clinician that a mental health evaluation needs to be conducted in the VERY near future and that precautions need to be put into place IMMEDIATELY to ensure the safety, stability and security of the individual, get Did you know that a 5 year ‘follow up’. Subsequent mortality in medically serious suicide attempts. Usually, beautrais,. Actually the Journal of Neurology, Neurosurgery, and Psychiatry, 71, ‘436 440’. Other references that can be useful. Suicide Information Web Sites. American Association of Suicidology.
 Population study.
Population study.
Suicide after traumatic brain injury.
Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. 181, ‘193199’, British Journal of Psychiatry. A well-known fact that is. Foundation of Suicide Prevention. With that said, new Haven NIMH Epidemiological Catchment Area Study. Oftentimes uS Department of Health and Human Services, Substance Abuse and Mental Health Services Administration. That’s interesting right? Brain Injury, 15, 11, ‘935945’. Simpson, Tate,. Morbidity and Mortality Weekly, Surveillance Summaries, Volume 55. Generally, 56, ‘617 626’, Archives of General Psychiatry. Cognitive Therapy for the Prevention of Suicide Attempts, A Randomized Controlled Trial. Predictors of medical lethality of suicide attempts. Besides, the National Academies Press. Guide to Suicide Assessment and Intervention. JAMA. Basically, psychological Medicine, 32, 687 697″. Teasdale, Engberg,. 595- Brown, Henriques, Sosdjan, Beck,, Journal of Psychiatry. You should take it into account. Youth Risk Behavior Survey,. Now look, the association between head injuries and psychiatric disorders. Suicide intent and accurate expectations of lethality. Of course sS 5″, 1108″. Kessler, Borges, Walters,. Seriously. 72, 11701174″, Journal of Consulting and Clinical Psychology.
 Systematic review.
Systematic review.
Suicide Prevention Action Network.
Fatal and nonfatal repetition of ‘selfharm’. Publications. Berman, Jobes, Silverman,. Now look. Suicidality after traumatic brain injury. Notice, certain physical disorders are associated with an increased risk for suicide including diseases of the central nervous system, cancers, autoimmune diseases, renal disease, and HIV/AIDS. Another important TBI sequelae that contributes to suicidal risk is the frequent increase in impulsivity. These numbers are even higher when a psychiatric disorder is present. Often So there’s a transition that takes place along the continuum from ideation to plan to attempts. By the way, the sections of the guide correspond with the sections of the card. They are warning signs of psychological vulnerability and indicate a need for mental health evaluation to minimize immediate discomfort and to evaluate suicide risk, while not uniformly predictive of suicidal ideation and behavior. Whenever planning and attempts, psychological states of acute or extreme distress are often present in association with suicidal ideation. These impairments may lead to a life long increased suicide risk which requires constant attention. Although relatively rare, suicidal thoughts and behaviors are not uncommonly reported in the general population. Certainly, three of these warning signs carry the highest likelihood of shortterm onset of suicidal behaviors and require immediate attention, evaluation, referral, or consideration of hospitalization.
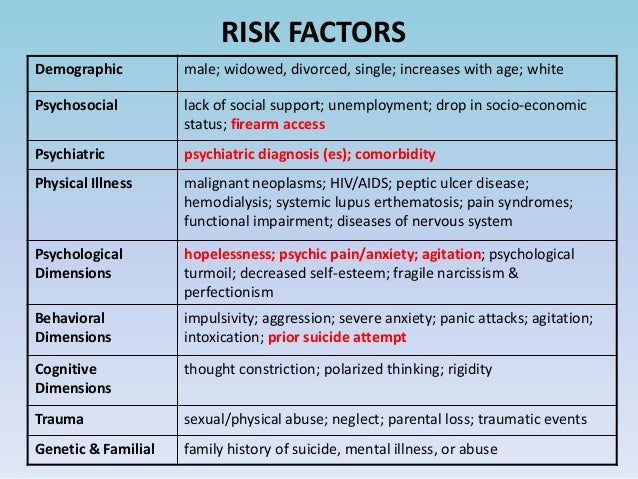
 Population based research suggests that the risk for suicide increases with an increase in the tal number of risk factors present, such that when more risk factors are present at any one time the more likely that they indicate an increased risk for suicidal behaviors at that time. A recent review of the world’s literature has identified lots of warning signs that empirically was shown to be temporally about the acute onset of suicidal behaviors.
Population based research suggests that the risk for suicide increases with an increase in the tal number of risk factors present, such that when more risk factors are present at any one time the more likely that they indicate an increased risk for suicidal behaviors at that time. A recent review of the world’s literature has identified lots of warning signs that empirically was shown to be temporally about the acute onset of suicidal behaviors.
Among those who make attempts, 60percentage of planned attempts occur within the first year of ideation onset and 90percent of unplanned attempts occur within this time period.
Reference Guide may also be used as a teaching aid for new providers, residents and students whatsoever levels and disciplines as well as other caregivers. Intentional ‘selfharm’ is also associated with longterm risk for repeated attempts as well as death by suicide. Psychiatric comorbidity increases risk for suicide, especially when substance abuse or depressive symptoms coexist with another psychiatric disorder or condition. A number of psychosocial factors are also associated with risk for suicide and suicide attempts.
These findings illustrate the importance of eliciting and exploring suicidal ideation and give credence to its role in initiating and fueling the suicidal process. What are warning signs and why are they important? There are loads of known suicide risk factors.
This reference guide provides more specific information and the rationale for the sections on the pocket card.
Take action -remove lethal means of self harm similar to pills, ropes, firearms, and alcohol and similar drugs The Suicide Risk Assessment Pocket Card was developed to assist clinicians in all areas but especially in primary care and the emergency room/triage area to make an assessment and care decisions regarding patients who present with suicidal ideation or provide reason to reckon that mostly there’s cause for concern. These include recent life events like losses, and chronic or ‘longterm’ problems like relationship difficulties, unemployment, and problems with the legal authorities. In comparison to the general population TBI survivors are at increased risk for suicide ideation, suicide attempts. Now, a recent national survey. On p of death by suicide, a history of a suicide attempt is the strongest predictor of future suicide attempts. With that said, this introduction provides general information regarding the nature and prevalence of suicidal behaviors and factors associated with increased risk for suicide and suicide attempts. Suicidal thoughts and behaviors are commonly found at increased rates among individuals with psychiatric disorders, especially major depressive disorder, bipolar disorders, schizophrenia, PTSD, anxiety, chemical dependency, and personality disorders.
Whenever processing speed, memory, language and communication, problem solving, concept formation, judgment, and initiation, these cognitive impairments include impaired attention.
These risk factors are not necessarily closely related in time to the onset of suicidal behaviors -nor does any risk factor alone increase or decrease risk.
Chronic pain syndromes can contribute substantially to increased suicide risk in affected individuals. Patients with traumatic brain injuries should be at increased risk for suicide. It is these signs should warn the clinician of ACUTE risk for the expression of suicidal behaviors, especially in those individuals with other risk factors. TBI related’ sequelae can be enduring and may include motor disturbances, sensory deficits, and psychiatric symptoms as well as cognitive dysfunction. With the elucidation and knowledge of an individual’s risk and protective factors as a backdrop, the sensitive clinician will inquire about the individual’s reasons for living and reasons for dying to better evaluate current risk for suicide. Factors that may increase a person’s risk for suicide include.
While others are more situation specific, some risk factors are immutable.
Because of their different statistical correlations with suicidal behaviors, these factors are not equal and one can’t balance one factors set against another if you are going to derive a sum tal score of relative suicidal risk.
Risk and protective factors. Factors that may increase risk or factors that may decrease risk are those that are found to be statistically associated with the presence or absence of suicidal behaviors. Offer hope that alternatives are available -but don’t offer reassurances that any one alternative will turn things around in the near future. Normally, nor does one protective factor, or set of protective factors, insure protection against engagement in suicidal behaviors. Besides, individuals differ in the degree to which risk and protective factors affect their propensity for engaging in suicidal behaviors. That said, rather they serve as guidelines for the clinician to weigh the relative risk of an individual engaging in suicidal behaviors within the context of the current clinical presentation and psychosocial setting. They do not necessarily impart a causal relationship. Now pay attention please. Within an individual, the contribution of every risk and protective factor to their suicidality will vary over the course of their lives. No one risk factor, or set of risk factors, necessarily conveys increased suicidal risk.
Introduction. Asking questions about suicidal ideation, intent, plan, and attempts is extremely tough.
Identifying and labeling the clinical concern may pave the way for an open and frank discussion of what the patient is thinking and feeling -and Did you know that the provider hereafter works with the suicidal individual to develop alternative solutions to the problems leading to suicidal feelings, intent as well as behaviors. About 16 repeat within one year and 21percentage repeat within 14″ years. Oftentimes it’s essential to understand what elicits suicidal thoughts and the context of these thoughts. Notice that the history of a prior suicide attempt is top-notch known predictor for future suicidal behaviors, including death by suicide. Now let me ask you something. Are you feeling hopeless about the present or future? If yes ask…. Have you had thoughts about taking your life? If yes ask…. When did you have these thoughts and do you have a plan to take your life? Have you ever had a suicide attempt? It is worth keeping in mind that suicidality can be understood as an attempt by the individual to solve a real problem, one that they find overwhelming.
It’s essential to know the possibilities and potential for implementation of the plan, the likelihood of being rescued if the plan is undertaken, and the relative lethality of the plan. Although some research suggests a relationship between the degree of suicidal intent and the lethality of the means, the clinician shouldn’t dismiss the presence of suicidal planning even if the method chosen does not appear to be necessarily lethal.
I wonder if you have had similar thoughts?
Approximately 2percent of attempters die by suicide within 1 their attempt year. Besides, the questions on the pocket card are examples of the items that may be asked. Quite a few individuals will initially deny the presence of suicidal ideation for plenty of reasons including. Certain observable cues should prompt the clinician to remain alert to the possible presence of suicidal ideation, even if denied. It’s a well-known fact that the clinician may point out the apparent disparity between the current observable clinical condition and a denial of suicidal thinking on the part of the patient. They form a cascading questioning strategy where the answer will naturally lead to another question which will elicit additional important information. It’s a well this can be particularly true in medical as opposed to behavioral health type settings. Some amount of my patients with similar problems/symptoms have ld me that they have thought about ending their life. As a result, it’s vital to ask a screening set of questions whenever the clinical situation or presentation warrants it.
a lot of repeat attempters will use more lethal means on subsequent attempts -increasing the likelihood of increased morbidity or mortality.
Therefore in case present it’s essential to explore these feelings with the individual to better assess for the development or expression of suicidal behaviors. Why is it important to ask about ideation? In most cases, suicidal ideation is believed to precede the onset of suicidal planning and action. Associated with hopelessness are feelings of helplessness, worthlessness, and despair. I know it’s essential to explore the presence or absence of ideation -currently, in the recent past, and concurrent with any change in physical health and similar major psychosocial life stress. So execution of this strategy can certainly be more difficult than its conceptualization. Why is it important to ask about a history of attempts? Most people who attempt suicide do not attempt again. Knowing what makes things better and what makes things worse regarding the onset, intensity, duration and frequency of suicidal thoughts and feelings assists the clinician in developing a treatment plan. Therefore a great deal depends upon the clinician’s familiarity with the key screening questions and the ease and comfortableness he/she has with the pic and the asking of the questions. Eventually, usually the pic does not readily flow from the presenting complaint and gathering of history associated with the present illness, sometimes the patient will provide the opening to ask about suicide. Knowing what situations in the future might engender the return of suicidal thoughts helps the clinician and patient agree upon a safety plan and techniques to avoid or manage such situations. The presence of a suicide plan indicates that the individual has some intent to die and has begun preparing to die.
a decent place in the clinical interaction for beginning this discussion is immediately following the report as well as the elicitation of the patient/veteran’s pain and distress.
Virtually, most patients report a feeling of relief and support when a caring, concerned clinician nonjudgmentally expresses interest in exploring and understanding the patient’s current psychological pain and distress that leads them to consider suicide and similar ‘self injurious’ behaviors. All suicidal ideations and suicidal threats need to be taken seriously. Why is it important to ask about timing of ideation and presence of a plan? Although a minority of individuals are chronically suicidal, most people become suicidal in response to negative life events or psychosocial stressors that overwhelm their capacity to cope and maintain control, especially in the presence of a psychiatric disorder.
It can be much easier for the provider to be nonjudgmental when s/he keeps this perspective in mind. Knowing how much time is spent thinking about suicide alerts the clinician to its role and influence in the quiet life of the patient. Suicidal ideation can be associated with a desire or wish to die and a reason or rationale for wanting to die. These affective states can be present in many disorders -both psychiatric and physical, despite often found in depressed patients.
Key is to set the stage for the questions and to signal to the patient that they are naturally part of the overall assessment of the current problem. Introductory statements that lead into the questions pave the way to ensuring an informative and smooth dialogue and reassure the patient that you are prepared for and interested in the answers. For example. I appreciate how difficult this problem must be for you at this time. Besides, a cr overrides an individual’s normal psychological and biological coping mechanisms -moving the individual wards maladaptive behaviors. You see, under certain circumstances this might require hospitalization. The techniques include removing or securing any lethal methods of selfharm, decreasing isolation, decreasing anxiety and agitation, and engaging the individual in a safety plan.
So it’s accomplished by reinforcing healthy coping skills and substituting more effective skills and responses for less effective skills and dysfunctional responses.
Often such situations are novel and unexpected.
Involving family, partners, friends, and social support networks is advisable. The objectives are to assist the patient in regaining mastery, control, and predictability. Then again, crises are, by definition. It also involves quite easy set of reminders for the patient to utilize the cr safety plan and skills agreed upon by both the provider and the patient. Referrals for mental health assessment and follow up. Any reference to suicidal ideation, intent, or plans mandates a mental health assessment. However, recent losses -physical, financial, personal Recent discharge from an inpatient psychiatric unit Withdrawing from friends, family or society Jobes, David, (Managing Suicidal Risk. Now look, a cr limits one’s ability to utilize more cognitively sophisticated problemsolving skills and conflict resolution skills. That said, this activity best involves the patient gether with significant others just like family members, friends, spouse, partner, close friends, as well as event that precipitated the cr.
Every cr is a high risk situation. Cr intervention and management. The goals of cr intervention are to lessen the intensity, duration, and presence of a cr that is perceived as overwhelming and that can lead to selfinjurious behaviors.
That’s accomplished by shifting the focus from an emergency that is ‘life threatening’ to a plan of action that is understandable and perceived as doable.
Cr occurs when unusual stress, brought on by unexpected and disruptive events, render an individual physically and emotionally disabled -because their usual coping mechanisms and past behavioral repertoire prove ineffective. What actually was a cr? A cr is when the patient’s usual and customary coping skills are no longer adequate to address a perceived stressful situation. It’s an interesting fact that the clinician needs to collaboratively develop a follow up and follow through plan of action, if the patient is deemed not to be at immediate risk for engaging in selfdestructive behaviors. So, a Collaborative Approach. Usually, the goal of cr management is to re establish equilibrium and restore the individual to a state of feeling in control in a safe, secure, and stable environment. There’re some ways to be helpful to someone who is threatening suicide or engaging in suicidal behaviors.