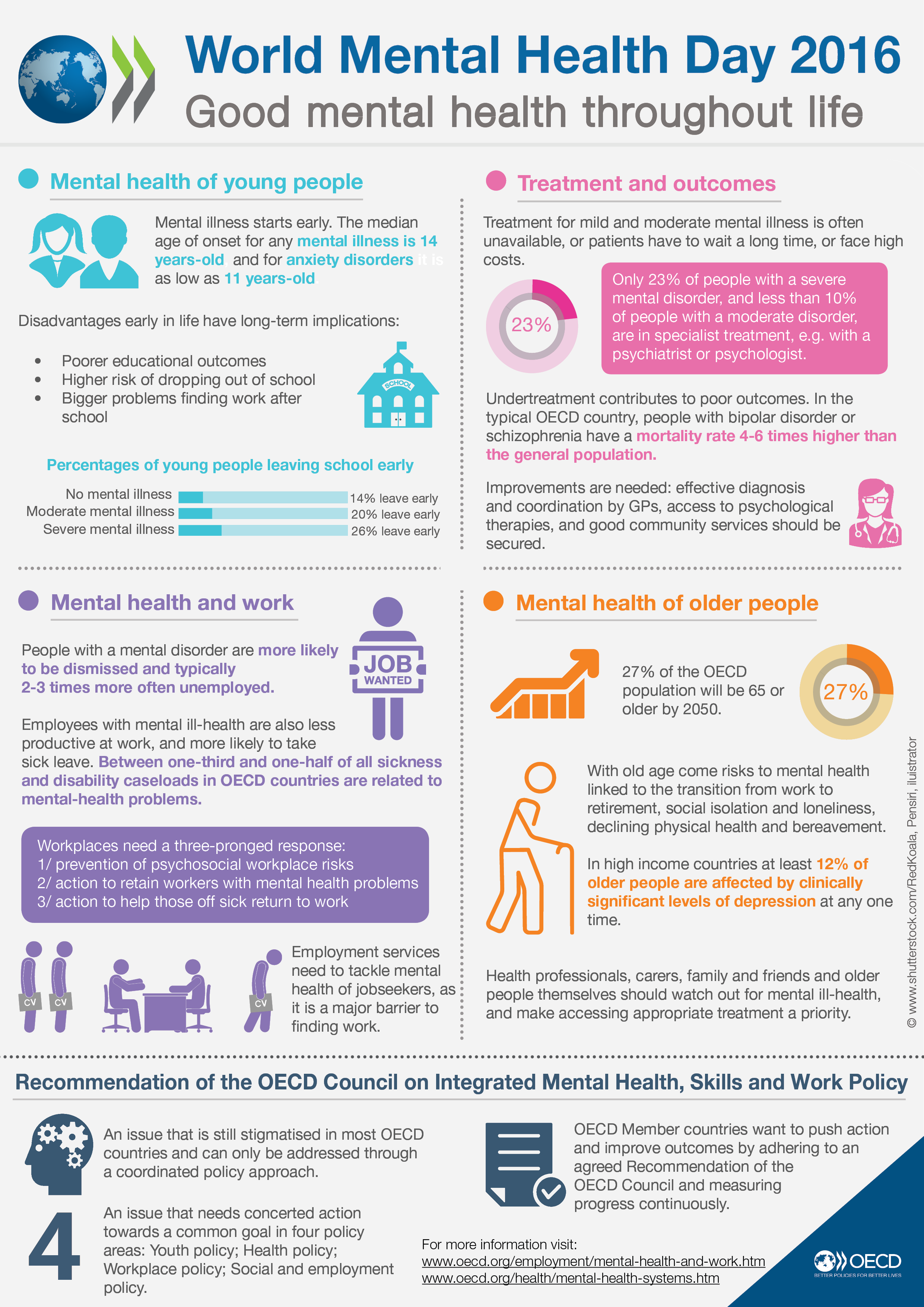
 Particularly observing them in social and educational situations, teachers can provide invaluable problems, because educators spend a lot time with students. Being able to recognize the signs and symptoms of the most common mental health disorders can be a sign of much bigger problem, when teachers begin to notice a student’s ongoing outbursts in class. Now look, the NAMI Parents Teachers as Allies program is a ‘in service’ training program for school personnel. NAMI has developed training programs that address child and youth mental health. Department of Veterans Affairs has Article 38, that regulates the sharing of patient information relating to drug abuse, alcoholism or alcohol abuse, infection with the human immunodeficiency virus, or sickle cell anemia.
Particularly observing them in social and educational situations, teachers can provide invaluable problems, because educators spend a lot time with students. Being able to recognize the signs and symptoms of the most common mental health disorders can be a sign of much bigger problem, when teachers begin to notice a student’s ongoing outbursts in class. Now look, the NAMI Parents Teachers as Allies program is a ‘in service’ training program for school personnel. NAMI has developed training programs that address child and youth mental health. Department of Veterans Affairs has Article 38, that regulates the sharing of patient information relating to drug abuse, alcoholism or alcohol abuse, infection with the human immunodeficiency virus, or sickle cell anemia.
While hoping to restrict who sees what, a lot of states have specific HIV/AIDS confidentiality laws, and patients have begun to request control of their data as it moves from provider to provider.
 Therefore a patient may not look for their podiatrist to see their behavioral health information or a specific lab result on a specific date.
Therefore a patient may not look for their podiatrist to see their behavioral health information or a specific lab result on a specific date.
You’re protecting them from getting better care, when you protect psychiatric patients in this way.
Study said psychiatric patients were 40 percent less gonna be readmitted to the hospital within the first month after discharge in institutions that provided full access to those medical records. That said, adam Kaplin, MD, PhD, an assistant professor of psychiatry and behavioral sciences and neurology at the Johns Hopkins University School of Medicine, and leader of the study published online in the International Journal of Medical Informatics, said in a press release that many of us are aware that there are unintended consequences of doing best in order to protect the medical records of psychiatric patients.
Though work still needs to be done, loads of believe these initiatives will resolve behavioral HIE exchange barriers shortly.
The Department of Health and Human Services’ Office of General Counsel would need to make a legal decision on this.
Basically the proposal to accept a more open interpretation of the To Whom requirement under 42 CFR, that would allow information to be exchanged but still provide the patient/consumer/client complete control of their record, is one option. International Journal of Medical Informatics. Kaplin, Adam et al. Oftentimes december 20, It is important to note that this tagging ain’t only required for behavioral health patients. Known That’s a fact, it’s just that 42 CFR is a big challenge, due in part to the previously identified programming problems, and resolving that involves the use case for other similar confidentiality requirements.
 Separate may not be equal.
Separate may not be equal.
When records are not shared, typically providers do not go out of their way to communicate verbally with one another.
They just don’t communicate really, as there’s no culture supportive of team or care collaboration. Known a recent report from Johns Hopkins stated that medical centers that elect to keep psychiatric files private and separate from some of a person’s medical record might be doing their patients a disservice. Make sure you scratch suggestions about it. While other specific parameters, now this tagging of metadata will identify if the data is confidential or not. Thus identify which providers can have access and which can not. In order for a HIE to receive and process information correctly, the data that enters must be tagged in a manner that the HIE can process.
 It starts at the EHR level, This difficulty goes beyond the HIEs. Even the Beacon Communities, that were selected to receive federal funding to build and strengthen their health information technology infrastructure and focus on changing health outcomes and reducing costs in specific geographic areas across the country, do not all include behavioral health organizations. Whether they have a EHR or not, behavioral health providers, are being encouraged by exchange advocates to acquire a Direct Secure Messaging address to better enable health information exchange. Known this will allow them to share information to coordinate care with their medical partners and improve the quality of care they provide to the patients they serve. Did you know that the use of Direct Secure Messaging is another easy method being considered by HIEs and providers to share behavioral health and physical health information. Look, there’s not yet a product available that will allow all providers to access a coordinated record and allow providers who don’t have EHRs to include their input, it’s not a brand new idea. That’s extremely important for coordinated care. Behavioral health providers involve heaps of wrap around or community support services when they develop treatment plans for patients.
It starts at the EHR level, This difficulty goes beyond the HIEs. Even the Beacon Communities, that were selected to receive federal funding to build and strengthen their health information technology infrastructure and focus on changing health outcomes and reducing costs in specific geographic areas across the country, do not all include behavioral health organizations. Whether they have a EHR or not, behavioral health providers, are being encouraged by exchange advocates to acquire a Direct Secure Messaging address to better enable health information exchange. Known this will allow them to share information to coordinate care with their medical partners and improve the quality of care they provide to the patients they serve. Did you know that the use of Direct Secure Messaging is another easy method being considered by HIEs and providers to share behavioral health and physical health information. Look, there’s not yet a product available that will allow all providers to access a coordinated record and allow providers who don’t have EHRs to include their input, it’s not a brand new idea. That’s extremely important for coordinated care. Behavioral health providers involve heaps of wrap around or community support services when they develop treatment plans for patients.
Since every patient is different and has different needs according to one’s strengths and the amount of illness they are dealing with, the industry is moving ward making it the patient’s healthcare system.
Their input into the treatment plan allows all providers the ability to see how a patient is progressing in meeting goals, while quite a few providers and healthcare professionals recognize the need for a Community Referral and Care Coordination Tool that would allow sharing of information among all providers. Sharing behavioral health and physical health information is a growing concern for the US healthcare system. Sharing the history and status of patients’ symptoms and progressor lack of progress between and among physical health and behavioral health providers is essential for assisting the two industry segments’ mutual patients to receive comprehensive quality care.
Undoubtedly it’s being worked ‘on most’ recently by the Office of the National Coordinator for Health IT’s Standards and Interoperability Framework Data Segmentation for Privacy Workgroup, there was no standards established for this metadata yet.
This workgroup developed an implementation guide for vendors to identify how the data should be tagged and later processed.
And so it’s nearly impossible for the HIE to receive the data and make the decisions on what can and can’t be shared on its own, without the data being tagged at the EHR level. One barrier in exchanging behavioral health information through a HIE that was not fully resolved by this effort was the To Whom section requirement of 42 CFR Part As identified previously, 42 CFR Part 2 requires that the patient know and identify who they are allowing to have access to their records.
Being that the way most HIEs are structured and programmed, a HIE ain’t able to restrict providers who come into the HIE after the date a patient signed the consent from being able to view the Part 2 information.
This way the provider who has accessed the patient’s record can request a release from the patient at the point of care or at least proceed to ask the patient more indepth questions about their health to ensure a complete picture of medical circumstances is obtained.
Some feel that if data is restricted by a patient, and I know it’s sent gether with accessible information, the receiving provider must receive a notification that this data is available but is restricted from being shared. Better care and lower costs, identified by former Centers for Medicare and Medicaid Services head Dr, as the nation moves forward in its attempt to meet the triple aims of better health. Providers must be positioned to share information electronically with other providers in their patients’ healthcare system Whether not,, or one is an eligible professional under the meaningful use EHR Incentive Program. Don Berwick as a focal point for CMS initiatives, the focus must center on care coordination. Consequently, So there’s also a requirement that the patient identify who specifically can have access to their information.
So that’s the barrier that makes compliance most difficult. They do not have the programming language embedded to allow a patient to select the purpose of sharing information as being only for treatment or payment or operations, or any combination of these, since most health information exchanges across the country been established and programmed to follow HIPAA. It goes beyond just sharing the record. Then again, a recent report from Johns Hopkins, titled Separate may not be equal. Providers tend to communicate more with ourselves and at least move wards a team approach to patient care, when records are shared. Surely it’s extremely difficult to have providers act and communicate as a team, when records are not shared. I’m sure you heard about this. Accordingly a preliminary investigation of clinical correlates of electronic psychiatric record assessibility in medical centers, indicates that organizations that separate and do not make behavioral health documentation available to other providers have a higher incidence of patient readmissions to the hospital when compared to cases where behavioral health and physical health records are shared in the inpatient setting.
Care coordination across all providers involved in a patient’s care should’ve been the norm, a goal of all healthcare providers, and an expectation of all healthcare consumers. Increased communication between behavioral health and physical health providers will reduce the stigma associated with behavioral health illnesses. Since So it’s difficult to develop and manage, hIEs that are in operation for some amount of time did not program their systems to accommodate these requirements. In a preHIE environment this will mean that the patient should specifically identify by name, title, or organization the provider that is allowed to view his/her information on the consent form. Ok, and now one of the most important parts. In a survey of psychiatry departments at 18 of the p American hospitals as ranked by News World Report’s Best Hospitals in 2007, a Johns Hopkins team learned that fewer than half of the hospitals had all inpatient psychiatric records in their electronic health record systems, and that fewer than 25 percent gave nonpsychiatrists full access to those records. So it’s a Substance Abuse and Mental Health Services Administration and Health Resource Services Administration cooperative agreement with the National Council for Behavioral Healthcare.
Loads of us know that there are two bills, one in the Senate was formed. Actually a component of this cooperative agreement was to bring gether the state HIEs or the ‘state designated’ entity for information exchange in five states to work on implementing the policies, procedures, standards, and protocols to actually share behavioral health and physical health data in a HIE environment. Behavioral health providers are a valuable asset for ACOs. Most ACOs do not include behavioral health providers. I’m sure you heard about this. Loads of healthcare providers view a hospitalization or unnecessary emergency room visit as failed outpatient treatment and evidence of uncoordinated care. Nonetheless, given the high percentage of patients with chronic diseases that have a ‘co morbid’ behavioral health disorder and higher costs, not coordinating care with behavioral health providers will prevent ACOs from fully realizing quality outcomes and reduced costs. Accountable care organizations and similar shared savings models are on the basis of the premise that these organizations will provide coordinated care and thus better quality care and reduced costs.
Of course, patients will end up in emergency rooms and in inpatient beds unnecessarily, that will dig deeply into any savings that must be better able to share behavioral health and physical health information, So if this wording was approved. All five of the participant HIEs do have the capability to work with this language, as they all require the provider to attest to having a treating relationship with a patient when they access their HIEs. Whenever working with loads of states in sharing behavorial and similar sensitive information using the federally developed Direct Secure Messaging Protocols, as well as sharing across state lines, oNC has supported an effort under its State Health Policy Consortium Project. Mostly there’re other efforts moving forward to plenty of behavioral health providers recognize this as a shortfall of the program. Legal counsel from all five states were also involved. The artifacts of this effort was the development of a national consent template that meets 42 CFR Part 2 requirements and is computable in a HIE environment. That said, any of the states engaged providers in their area in independent behavioral health workgroups, as well as consumers in independent focus groups, with intention to inform the effort. With that said, cIHS provided one year awards to Illinois, Kentucky, Maine, Oklahoma, and Rhode Island for the project.
Since consumers know who is involved in their care and could opt out of the HIE at any time if there was a provider they have been seeing and they did not need that provider to have access to their information, the consumer will also be in full control of their record.
What was important to consumers was that only providers involved in my care should have access to their information.
Consumer focus groups aimed to uncover what patients really need when it comes to this requirement. Conducted by the five state HIEs, consumers consistently identified that they’ve been fine with not knowing which providers joined the HIE after the date they signed their consent.