Many of us have come throughout analysis that tracks patterns of mental health issues throughout childhood and adolescence. Such analysis asks questions like: what quantity of the inhabitants expertise mental health issues throughout childhood? What sub-groups can be recognized? And what number of people with a mental health downside worsen, enhance or keep the identical over time?
Historically, longitudinal cohort research such because the Dunedin research in New Zealand (Caspi et al., 2020) and ALSPAC within the UK (McElroy et al., 2017) have been the bread and butter of this sort of analysis. In 2022, I used to be additionally concerned in a research that used two longitudinal cohorts in Ireland to establish trajectories of signs throughout childhood (Healy et al., 2022).
However, a nagging query that plagues us all who use such datasets is: do longitudinal cohort research seize “real life”? There is at all times the likelihood that the people in these cohorts are a biased group—self-selected to be obtainable and keen to take part, or “contaminated” considerably by the repeated questioning throughout their lives.
The research being reviewed right here has used real-life healthcare information to have a look at how younger folks work together with healthcare providers for mental health assist.

Do potential research actually tell us a lot about the real-life use of healthcare? This research makes use of GP records to evaluate ‘real world’ use of healthcare providers for mental health assist in younger folks.
Methods
This research used the CPRD-Aurum system (which captures on a regular basis data from 25% of GP practices throughout England), and two different information registers: Hospital Episode Statistics and Office for National Statistics. The pattern included all sufferers aged 3-18 who introduced to their GP with a mental health downside between 2000 and 2016. To be included within the research, the clinician should have included a code for a mental health symptom or analysis within the affected person notes at that appointment.
The predominant intention was to group collectively people who confirmed comparable patterns of (1) GP attendance, (2) prescriptions, and (3) contact with specialist mental health providers, over the following 5 years. These teams have been chosen utilizing group-based multi-trajectory modelling.
Results
369,340 people have been recognized as eligible from the first care records. The authors discovered that 7 teams finest captured several types of service-use on this pattern within the 5 years after their preliminary presentation (see determine).
Just over half of the pattern fell into group 1, who have been characterised by low GP contact (after that preliminary presentation), low numbers of prescription medicines, and little contact with specialist providers.
The particulars of all different teams can be seen in Figure A. But I’ll draw consideration to three key findings right here:
- There have been simply 2 teams with persistently excessive prescriptions (teams 6 and seven) which made up ~15% of the pattern. Over 60% of those people had been prescribed remedy at their preliminary mental health presentation, rising to 80% in subsequent years. This group additionally confirmed comparatively secure GP contact throughout the 5-year follow-up, with 40-50% of group 6 and 60-70% of group 7 seeing their GP annually.
- Some intercourse variations may very well be noticed in groupings. For occasion, females made up 60% of teams 3 and 5, which have been characterised by excessive charges of despair and nervousness. Conversely, there was a slight majority (57%) of males in group 2, who have been characterised by youthful age at presentation, with points corresponding to autism, behavioural and conduct issues. However, these intercourse variations wouldn’t warrant labelling any group as a “male” or “female” group.
- For teams 3, 4 and 5, there have been drastic adjustments in service use throughout the 5-year interval. Group 3 noticed a stepwise drop in all kinds of service-use annually after preliminary presentation. It is troublesome to know whether or not this displays enhancing mental health, or rising dissatisfaction with providers. Groups 4 and 5 alternatively noticed sharp will increase in GP contact and prescriptions a number of years after the preliminary presentation. Similarly, it’s troublesome to know whether or not these delayed escalations in service use replicate preliminary misdiagnosis, ineffective remedy, or just a worsening of signs resulting from non-healthcare components (e.g. hostile life experiences).
Finally, the authors investigated whether or not membership of any of those teams predicted time to (a) hospital admission for self-harm or (b) loss of life by suicide. The majority group (low contact with providers) was used because the reference group. Even after adjustment for potential confounds, most teams confirmed a considerably elevated danger of those two severe outcomes. The exception throughout each outcomes was group 3 who have been characterised by the year-on-year drop in service use.
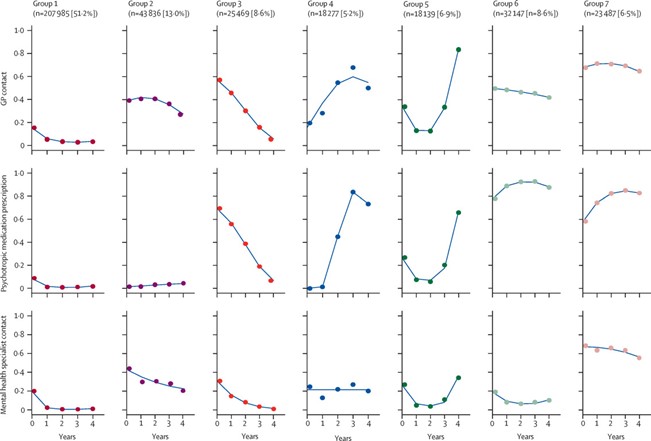
This research discovered that younger individuals who contacted their GP for mental health assist between the ages of three and 16 fell into one among seven teams, with over half of the pattern being categorised by low engagement with GP, specialist providers and prescriptions following preliminary presentation. [View full sized graphic]
Conclusions
The authors conclude that their findings could reassure youngsters, adolescents & caregivers as a result of 51.2% of kids who introduced to their GP with a mental health challenge went on to have low contact with providers. One would possibly argue that this reassuring majority additionally contains group 3 (8.6%), who had lowering service use over the 5-year interval, and weren’t considerably completely different from the low-contact group when it comes to subsequent danger of self-harm or suicide in adjusted fashions.
However, the authors emphasise that these outcomes replicate service-use solely. It stays troublesome to say whether or not low contact with providers displays higher mental health or disengagement with providers resulting from unmet wants.

These findings could ‘reassure’ youngsters, adolescents and caregivers on condition that 51.2% of kids who introduced to their GP with a mental health challenge went on to have low contact with providers.
Strengths and limitations
The main worth of this research lies in its use of real-life major care information, nonetheless that is additionally its predominant limitation.
One available, this research has energy in numbers resulting from its use of a nationwide major care database (CPRD-Aurum). It additionally has energy in ecological validity (avoids some choice biases) and scientific validity (all members sought assist for a mental health downside, arguably capturing non-trivial signs or practical impairment).
On the opposite hand, we may ask: who’s actually captured on this pattern of kids who’ve introduced to their GP for a mental health challenge? The reply might be a sophisticated one involving the visibility of the kid’s mental health challenge, the child-carer relationship, stigma round mental health, belief in healthcare providers and entry.
Results from the Mental Health of Children & Young People in England survey (2021) confirmed that 1 in 4 mother and father don’t search skilled assist/recommendation for his or her little one (aged 6-16) even when that little one has a possible mental health dysfunction. The similar survey additionally confirmed that lower than half of older adolescents (and people of their early 20s) with mental health points are prone to search assist in health providers. Therefore, we may argue that this research pattern could also be biased towards those that have entry to a GP service, really feel comfy presenting with a mental health challenge, and towards mental health points that are extra seen or understood.
There are a number of different limitations of this research price contemplating that the authors didn’t point out:
- Data-driven trajectories: In the statistics part of the paper, the authors clarify how they examined various fashions with 1-7 teams to see which one confirmed the perfect match to the information. The most variety of teams (7) confirmed the perfect match to the information which raises the query: whereas it’d paint a extra complicated image, is the variety of teams that finest seize the information better than 7?
- Missed kinds of care: Specialist mental health care included “contact with psychiatrists, psychologists, or child and adolescent mental health services [CAMHS], or referrals for psychiatric symptoms or diagnoses”. But what’s lacking right here? I puzzled whether or not referrals from faculties to CAMHS or incapacity providers could be captured within the major care system. Also lacking from this listing of specialist assist are non-public counsellors together with these accessed by way of net suppliers like BetterHelp, which have risen in reputation amongst adolescents (Ineqe Group, 2022)

The use of real-life major care information is each a energy and limitation of this research.
Implications for observe
One of the important thing implications of this research is how routine GP information may very well be used to predict the care wants of an adolescent at preliminary presentation. There are each monetary and health incentives to establish who would require intensive assist forward of time, and to curb service overload by delivering earlier or extra applicable intervention to those that want it. At a time when NHS mental health providers are stretched, all efforts to make the system extra environment friendly are worthwhile. However, my guess is that the authors didn’t point out this implication as a result of there may be fairly a big piece of labor to be accomplished to increase these findings into correct prediction modelling.
Another implication of this work for health service evaluators is the potential for specialised mental health assist to alleviate the strain on major care clinics. The outcomes of this paper and others (Kontopantelis et al., 2021; NHS England, 2024) counsel {that a} small variety of folks could account for a disproportionate variety of GP appointments. Take group 7 as an illustration: ~70% of those people attend their GP annually with a mental health associated challenge. Is the GP clinic the perfect type of assist for these people? Could a specialised youth mental health service serve two functions by (1) relieving strain on GP providers and (2) offering extra specialised assist to those younger folks? Such fashions of youth assist are already in operation in Australia (e.g. Headspace) and Canada (e.g. Youth Wellness Hubs).
The authors notice that extra analysis must be accomplished to complement findings like these from health registers with extra granular data on affected person signs and functioning. I might add that qualitative enter or affected person and public engagement from younger folks (or their carers) who’ve sought assist from their GPs for his or her mental health must be built-in with this sort of information to really perceive how providers work for this group.

Is the GP clinic the perfect type of assist for younger folks experiencing recurrent mental health points?
Statement of pursuits
No conflicts of curiosity to reveal.
Links
Primary paper
Senior M, Pierce M, Taxiarchi VP, et al. 5-year mental health outcomes for kids and adolescents presenting with psychiatric signs to normal practitioners in England: a retrospective cohort research. The Lancet Psychiatry. 2024;11(4):274-284.
Other references
Caspi, A., Houts, R. M., Ambler, A., Danese, A., Elliott, M. L., Hariri, A., Harrington, H., Hogan, S., Poulton, R., Ramrakha, S., Rasmussen, L. J. H., Reuben, A., Richmond-Rakerd, L., Sugden, Ok., Wertz, J., Williams, B. S. & Moffitt, T. E. (2020). Longitudinal Assessment of Mental Health Disorders and Comorbidities Across 4 Decades Among Participants within the Dunedin Birth Cohort Study. JAMA Netw Open 3, e203221.
Healy, C., Brannigan, R., Dooley, N., Staines, L., Keeley, H., Whelan, R., Clarke, M., Zammit, S., Kelleher, I. & Cannon, M. (2022). Person-Centered Trajectories of Psychopathology From Early Childhood to Late Adolescence. JAMA Netw Open 5, e229601.
Kontopantelis, E., Panagioti, M., Farragher, T., Munford, L. A., Parisi, R., Planner, C., Spooner, S., Tse, A., Ashcroft, D. M. & Esmail, A. (2021). Consultation patterns and frequent attenders in UK major care from 2000 to 2019: a retrospective cohort evaluation of session occasions throughout 845 normal practices. BMJ Open 11, e054666.
McElroy, E., Shevlin, M. & Murphy, J. (2017). Internalizing and externalizing issues in childhood and adolescence: A latent transition evaluation utilizing ALSPAC information. Comprehensive Psychiatry 75, 75-84.
NHS England (2024). News article: Two million extra GP appointments for sufferers than earlier than the pandemic. Published 15 Feb 2024.